(12-12-17) I’m in Richmond today participating in a meeting about mental health priorities for incoming Virginia Governor Ralph Northam. Meanwhile, I want to share a study being released today.
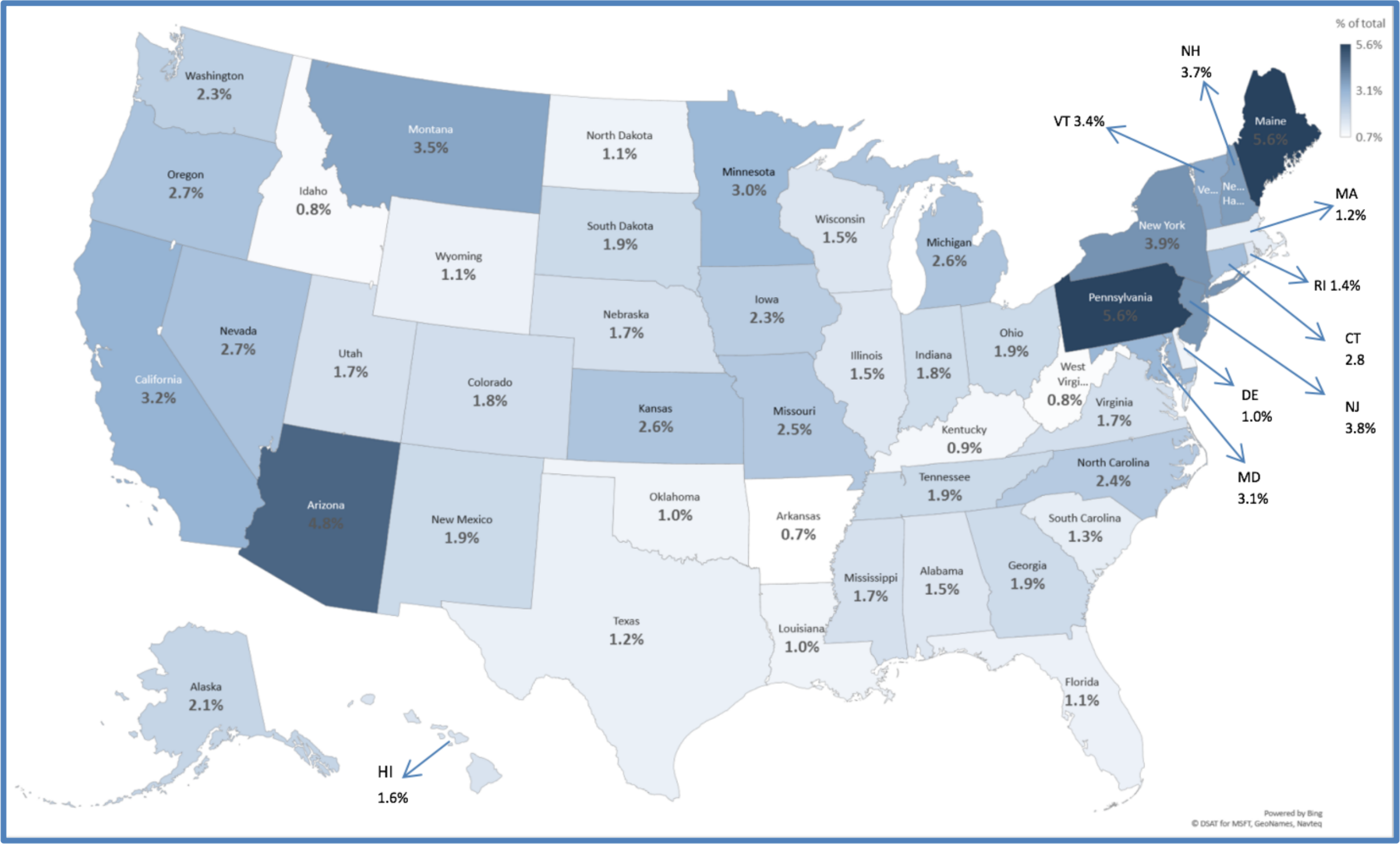
New Study Reveals Shameful Eight-Fold Difference in Percentage of State Funds Allocated to Helping Mentally Ill.
- Maine, Pennsylvania and Arizona are the most generous states.
- Arkansas, West Virginia, Idaho, Kentucky, Oklahoma, Louisiana and Delaware are the stingiest states.
Mental Illness Policy Org just released the first study to rank all fifty states based on the percentage of state-controlled funds that each state spends on mental illness. States that spend a higher percentage of their overall budget on mental illness are ranked as generous and those that spend a lower percentage of their overall budget on mental illness are ranked as stingy. Put another way, this report describes which states have been “naughty or nice” to the mentally ill.
Funds for Mental Illness found the most generous states in mental health spending are Maine, Pennsylvania and Arizona. The stingiest states are Arkansas, West Virginia, Idaho, Kentucky, Oklahoma, Louisiana and Delaware. The most generous states, Maine and Pennsylvania (5.6%), allocate eight times more as a percentage of total state spending than the stingiest state, Arkansas (.7%).