“There is a huge portion of our community that doesn’t necessarily want two officers showing up when they call about a situation with respect to behavioral and mental health,” the mayor said in an interview Sunday. “So this is a new path forward for us that has been illuminated because of what we’ve learned during these times. Look, there’s political will; there was not political will to make this huge of a step three weeks ago.”
New Mexico City To Develop Non-Police Response To Mental Health Calls – Homeless Issues
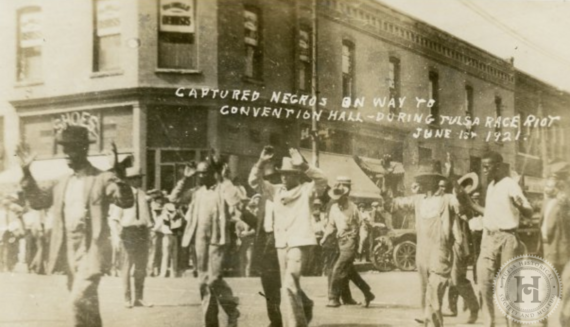
Tulsa Race Riot: Back In 1982, Young Author Told Me About What Happened That Day
Tulsa Historical Society photo.
THIS IS NOT ABOUT MENTAL HEALTH
(6-15-20) Back in 1982, I interviewed Scott Ellsworth, then a young doctoral candidate who’d written a book about the 1921 race riot in Tulsa. As a child, I lived for several years in Oklahoma, graduated from college there, and ultimately worked at the now-closed The Tulsa Tribune newspaper. Because of my Oklahoma ties, I convinced my editors at The Washington Post to let me write a story about Ellsworth’s book, Death in a Promised Land, the first definitive account about that horrific massacre.
The Untold Story of One of America’s Worst Race Riot
BILL WILLIAMS once asked his father why he had come to Oklahoma. “Well,” the old man replied, “I came out to the promised land.”
During the early 1900s, Oklahoma had become a land of opportunity for blacks. Tulsa in particular had developed a thriving black business district that had become so prosperous that in 1913 it was known nationally as the Negro’s Wall Street.”
The Williams family had played a major role in making that black business district successful. Bill’s parents, John and Loula, had come to Oklahoma in 1902 when the area was still known as Indian Territory. They were looking for a place to settle and Tulsa seemed like a prime spot. Jobs were plentiful in the oil boom town. Fortunes were made and lost in a single day. By 1920, the Williams were among the richest black families in Tulsa. They owned a garage, confectionary, boarding house and the first movie house for blacks in the city. They called it the Williams Dreamland Theatre.
On the night of May 31, 1921, all that began to change. The land of promise turned ugly for blacks. Bill Williams, who was 16 at the time, remembers waking to the sounds of gunshots. His father was firing out their apartment window at a gang of white men who were trying to break into the building and loot it.
During the next 24 hours, Tulsa experienced one of this nation’s worst race riots. An estimated 270 persons, including some of the city’s most prominent blacks, were killed. More than 1,000 homes owned by black families were destroyed. The black business district was devastated.
Dealing With Mental Illnesses Should Be A Medical Issue Not A Police Problem

(6-15-20) In an opinion editorial published by the Washington Post today, I call for shifting responsibility for the seriously mentally ill away from the police to community social services and the medical community.
Mental Illness Is A Health Issue, Not A Police Issue
(Reprinted From The Washington Post)
By Pete Earley
Pete Earley is the parent designee on the Interdepartmental Serious Mental Illness Coordinating Committee, which advises the federal government about mental health reform.
Americans with mental illnesses make up nearly a quarter of those killed by police officers, according to The Post’s Fatal Force database. Meanwhile, a cumulative list shows 115 police officers have been killed since the 1970s by individuals with untreated serious mental illnesses.
It doesn’t have to be this way. The movement underway to “defund the police,” is a long-needed moment to shift responsibility for the seriously mentally ill away from police and put it back to where it belongs: on social service agencies and the medical community.
Forty percent of adults with serious mental illnesses will come into contact with the criminal justice system during their lives. Each year, 2 million of them are booked into jails. Most are charged with minor misdemeanor crimes and low-level felonies directly tied to their psychiatric illnesses. Jails and prisons currently hold more people with serious mental illnesses — 365,000 individuals — than hospitals. They remain in jail four to eight times longer than people without mental illnesses charged with the exact same crime, cost seven times more than other inmates in jail, are less likely to make bail and more likely to gain new charges while incarcerated.
Charges Against Fairfax Officer In Taser Incident Wouldn’t Have Happened Without Public Outcry About 2 Earlier Deaths
(6-11-20) Millions of Americans have watched bodycam video of a white Fairfax County (Va.) police officer fire a stun gun probe into an unarmed, clearly disoriented black man before pinning him to the pavement, striking him with the stun gun and apparently firing another jolt to subdue him.
Fairfax Police Chief Edwin C. Roessler Jr., and Commonwealth Attorney Steve Descano immediately condemned Officer Tyler Timberlake’s actions. Roessler called the officer’s conduct “horrible” and “disgusting,” adding “What you see here is unacceptable. It does not value the sanctity of human life.”
Timberlake was charged with three misdemeanor counts of assault and battery.
To fully understand the refreshing importance of Roessler’s and Descano’s actions, you must look backward at two earlier deaths at the hands of Fairfax law enforcement.
Federal Govt. Accused Of Abandoning Research That Would Provide Short Term Help To The Most Seriously Mentally Ill

Dr. E. Fuller Torrey rips into NIMH, its advisory board and NAMI
(6-8-20) Dr. E. Fuller Torrey is again accusing the National Institutes of Mental Health of virtually abandoning clinical trials that could help Americans with schizophrenia and bipolar disorder in the short term.
Instead, NIMH, the main federal government agency for research into mental illness with a budget of almost $2 billion, has made basic brain research its priority. The results of such research will take three or four decades to show results, if then.
What’s the difference between “clinical trials” and “basic research.”
Elizabeth Sinclair Hancq, the director of research at the Treatment Advocacy Agency, which Dr. Torrey helped found, provided examples for me in an email.
- Basic research: growing cells in petri dishes and testing the effect of a particular drug on cellular mechanisms, like stopping their growth or activity. Basic research also includes animal model studies when trying to understand underlying cellular or system biology.
- Clinical trials: Testing the effect of a particular drug on symptoms and disease processes.
Perhaps the best way to see the marked difference between the two is by looking at clinical trials the NIMH is not funding. TAC listed 16 examples in a press release all of which are listed at the end of this blog.
Here is a sampling:
- Efficacy of generic drugs: Psychiatric patients being switched from brand-name to generic psychiatric medications frequently complain about loss of efficacy. NIMH should support studies of generic drug efficacy for psychiatric illnesses.
- Long-term injectable antipsychotics: In recent years, several new long-term injectable antipsychotics have been introduced. Although each was approved by the FDA for being better than a placebo, almost nothing is known about their comparative efficacy against each other. NIMH funded trials on these medications would help physicians make more informed decisions on medications for their patients.
- Long term effects: Many of the psychotropic drugs commonly administered to millions of patients in the United States were only studied for their acute effects. Very little is known about the long-term effects of treatment with these medications regarding side effects, maintenance dose, and use of blood levels. These should be systematically studied. The results of such studies might enable treatment using doses which are lower than those currently used, reducing side effects and improving medication compliance.
- Duration of treatment: Current guidelines are not clear regarding how long patients should be treated after a first episode of psychosis. In practice, many clinicians recommend stopping after one year, often increasing risk of relapse. (Studies) should be done randomizing patients to continuation of low dose antipsychotic treatment 1, 2 and three years after their first psychotic episode, to see if continued treatment reduces risk of relapse, while monitoring side effects.
- ECT: Electroconvulsive therapy (ECT) is underused in the United States compared to other developed nations. Randomized, sham–controlled studies using modern research designs should be conducted in the United States testing the efficacy and safety of ECT. This might encourage the use of this unpopular, but safe and efficacious evidence-based treatment.
Dr. Torrey wrote that NIMH funding is now skewed with 90 percent going for basic research, versus a fifty-fifty split.
A Blueprint For Making The Mental Health Movement More Relevant and Effective

(6-5-20) From My Files Friday: In 2016, I asked Washington area management consultant Steven Kussmann to suggest ways the mental health community could be more effective in achieving meaningful reforms. Given all that is happening in our nation now, his call for action seems especially appropriate.
Changing The Mental Health Movement From Within
by Steven Kussmann
Less than 3% of our population self-identifies as gay or lesbian. Yet, the LGBT community created a movement that changed our nation’s definition of marriage and secured same sex marriage as a constitutional right! Change did not happen organically nor overnight. It was the result of a highly-effective social movement strategy and decades of well-targeted action.
The number of U.S. citizens with a serious emotional and mental health disorder is 10-times greater than the LGBT population. Why then do our social and political successes pale in comparison with those achieved by this community? What can we learn from them to achieve similar results? How can we apply those lessons to transform the mental health movement into a powerful engine for effective change?
The lessons are many, and their application requires a fundamental refocus of movement strategy and structure. To succeed as a force for real social and political change, the mental health community, both its leadership and grassroots network, must rethink and retool its strategy and tactics.
Here are five get-the-ball-rolling ‘lessons learned’ from the success of others the mental health community can act on now: