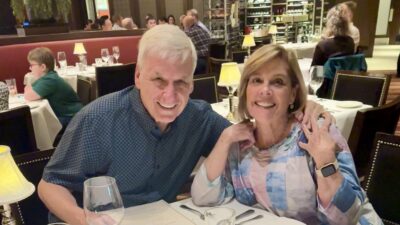
Kevin and I spoke at a Washington D.C. mental health fundraiser – a few years ago in black tie near the White House
(1-22-26) I’m proud that my son, Kevin (known as Michael in my book), posted his first blog on this website today. Look for the tab that says: Kevin’s blog.
I’ve encouraged him to write about his mental illness, his recovery, and his work as a certified peer and recovery specialist. I happily pass the “blog baton” to him as I continue to focus on my health and family. I will be curious to read his thoughts. I hope you will be too.
Thank you for your continued support and dedication to reforming our mental health system.