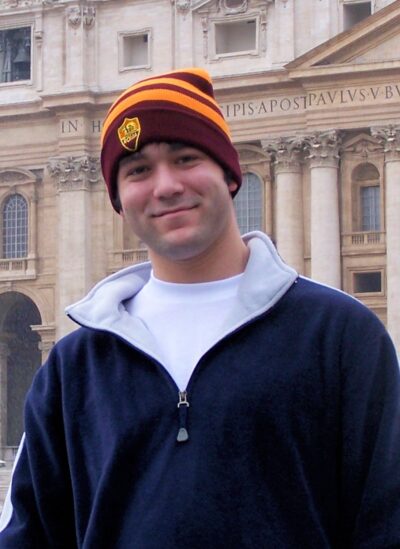
Matthew Milam’s parents sued hospital after doctors ignored warning signs their son was suicidal. No one listened. (Photo courtesy of Pat and Debbie Milam)
(12-15-23) Pat Milam was desperate. He knew his adult son, Matthew, was planning on killing himself. But doctors at the Ochsner Hospital/Clinic where his hospitalized son was being treated for bipolar disorder and paranoid sczhophrenia weren’t listening.
The more Pat tried to sound alarms, the more doctors at the large medical center on the outskirts of New Orleans, La., balked. One said he didn’t want to “upset” Matthew by sharing his father’s worries. But mostly, Pat and his wife, Debbie, were told the federal Health Insurance Portability and Accountability Act (HIPAA) prevented the hospital from discussing Matthew’s case.
“I told them, you don’t need to tell me a damn thing about my son,” Pat recalled in a telephone call. “I know my son. You need to let me tell you about what is happening on the other side” – at home.
“I took photos of Matthew standing in a thunderstorm begging God to strike him down by lightening,” Pat explained, hoping to substantiate his fears. “I got a notarized affidavit from a co-worker who described how Matthew had showed him a noose and said he was going to use it to kill himself. I documented how Matthew had dug his own grave in our backyard and had slashed his throat.” Pat went so far as to get a letter a psychiatrist not affiliated with Ochsner stating that Pat was not an “alarmist” but had reasons to be worried.
Pat hand-delivered all of those documents to Ochsner. Despite this, he was told that Matthew would be discharged. Doctors said he was stable. Pat contacted the CEO of Ochsner and begged him to intervene – as one parent to another. No one listened.
Eight days after being sent home, Matthew was dead at age 24.
Grieving, heartbroken and angry, Pat sued Ochsner Medical Institutions, one of the largest providers in the South. It was a David vs Goliath challenge – Ochsner is a four billion dollar operation with 30,000 employees.
Now, twelve years after Matthew’s suicide and despite repeated attempts by Ochsner lawyers to drag out the couple’s civil suit, depose them with embarrassing questions about their personal lives, and drive up attorney bills, Pat and Debbie reached a settlement.







