Matt Milam, another casualty
FROM MY FILES FRIDAY — This blog post, which I published last year, led to Pat Milam being invited to testify before a congressional subcommittee about the difficulties that families face when trying to help a loved one who has a mental disorder. I’m happy to report that Pat has continued with his advocacy since that hearing in a tireless effort to turn a spotlight on the Health Insurance and Portability Accountability Act (HIPAA) and how some doctors use it avoid talking to family members. Partly because of Pat, Rep. Tim Murphy held a community meeting in Pittsburg to further examine HIPAA. At that hearing, Charles and Debi Mahoney described the suicide death of their college age son, Chuck. They said HIPAA kept school officials from telling them information that might have helped save Chuck’s life.
What’s your take on HIPAA? Does it do more harm than good? Should there be an exemption when the patient has a mental disorder? Is it important to protecting the privacy of someone with a mental disorder? Good or bad — please share your story with us.
And thanks Republican Rep. Murphy for continuing to hold hearings about our troubled mental health care system.
A FATHER GRIEVES, NO ONE LISTENED TO THE PARENTS
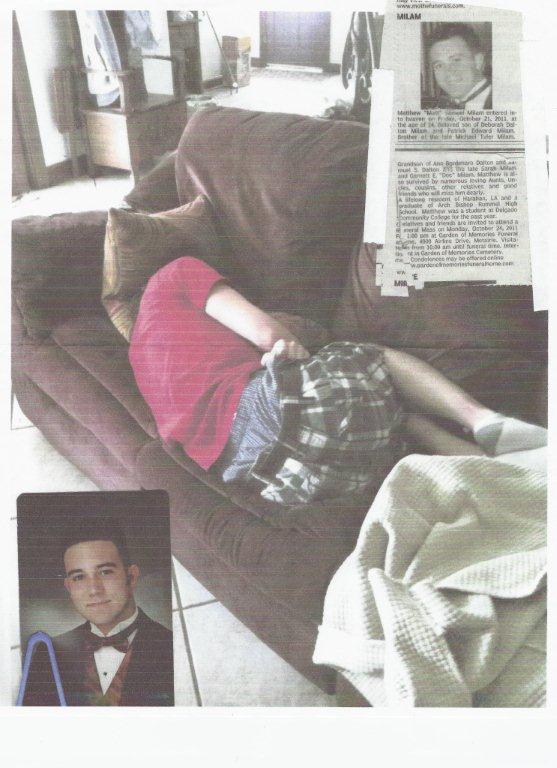
Pat Milam knows what it is like to bury a child. But it was not a gunman who murdered his son in October 2011. It was America’s failed mental health system, the still-grieving father says.
Pat and Debbie Milam’s twenty-four year old son, Matthew, ended his own life eight days after he was discharged from a psychiatric ward in New Orleans, Louisiana, where he was being treated for bi-polar disorder and paranoid schizophrenia – although his parents have a difficult time actually calling what happened comprehensive “treatment.” Pat calls it “stabilize and release.” They claim Matthew was hustled through a system that did little to actually help their son while their repeatedly pleas for help were ignored.

“My son slashed his own throat,” Pat says. “He dug a grave in our backyard and told us that’s where he wanted to be buried when he killed himself. He showed his friends nooses that he’d made to hang himself, hid gasoline, propane tanks and rat poison inside his bedroom closet and attacked my wife, threw a cell phone at her and broke apart a pair of scissors and said he would kill us both and put our blood on the wall. But doctors would not discuss anything with us when we warned them that he was suicidal!”
Pat claims the doctors treating his son didn’t tell the family information about his son’s care because restrictions mandated by the Health Insurance Portability and Accountability Act (HIPAA.), even though Pat and Debbie sent frequent one way updates to Matt’s doctors. After his son’s death, Pat obtained copies of his son’s medical records and discovered that Matt had signed a wavier authorizing doctors to discuss his case with his parents. Matt’s primary psych doctor evidently didn’t care or was worn out, Pat says, “regardless, we never got a call…No one wanted to tell us anything. They would not communicate with us and Matt’s doctor certainly didn’t tell us that he thought our son was suicidal.”
According to medical records the Milam’s now have, Matt’s primary psychiatrist noted that Matt was “at a high risk for suicide or other bad outcome” three months before his death. Pat says the doctor didn’t warn him or his wife about Matt being dangerous even though he was living with them in their home at the time.
On June 14, 2011, Matt drove to an emergency room and told doctors that his “brain was leaking.” He demanded a brain scan. The scan failed to detect a lesion or leakage, but the doctors there noted in their report that Matt appeared to be paranoid and delusional. Matt even asked the doctors to prove they were really doctors. He was sent home without treatment.
Not long after that, Pat discovered Matt in the family’s backyard digging a grave. “He said it was where he wanted to be buried after he killed himself.”
Pat sent Matt’s psychiatrist another note about this and again got no response- although the doctor did discuss the grave with Matt, Pat found out later in the medical records. A month later, Matt slashed his own throat while talking to his mother in the kitchen. He’d lost nearly two liters of blood by the time he was admitted into the hospital. He told doctors he’d hurt himself because “men in a black car” that drove past their house were after him. Matt stayed at the hospital in a locked ward a few days, took his meds, did better and was discharged back to his primary psych care physician.
A few weeks after he was discharged, Matt’s primary psychiatrist noted in medical records after meeting with Matt that his “progress was bumpy.” The psychiatrist wrote that Matt remained an “extremely high… risk for suicide or other bad outcome.” But the doctor never communicated this to Pat and Debbie.
A month later, Matt’s psychiatrist wrote that his patient showed signs of “hypo-manic activity…his mind just goes from one thing to the next.” Matt had told the doctor the “Sumerians were visited by the aliens.”
His parents became alarmed again when Pat spotted their son standing outside during a violent thunderstorm. He was begging God to strike him with lightening. Pat snapped a picture of his son in the lightning storm for his son’s psychiatrist. He was worried Matt might be able to deny or explain his bizarre behavior. “I sent the photo to his doctor and again nothing happened.”
Matt’s behavior turned violent shortly after the thunderstorm incident. This time, he broke a pair of scissors and threatened to “kill his parents and put their blood on the wall.” He accused his mother of being the devil. Pat called the police again. They came and talked to Matt. They left after he assured them that he’d calmed down. They thought Matt was throwing a fit because he wanted his parents to give him money to go to a school fair. It should be noted Pat owned guns and had removed them from the property years before.
On Oct. 5th, Matt called home drunk and told his parents that someone had stolen his car. Pat suspected his son, who had a drug problem in the past but was now clean, had either traded the car for drugs or money or had given it away because he planned to kill himself. Pat admits that he was terrified about suicide, in part, because Matt’s younger brother had died from a drug overdose a few years earlier. He didn’t want to lose Matt too.
Increasingly concerned about his son’s behavior, Pat decided to inspect his son’s bedroom when Matt left the house to take the family dog on a walk. Inside a closet, he found two gallon gasoline cans with petrol, large BBQ size propane tanks, flares, a propane torch, rat poison and a shotgun shell. Pat called the police again, and the police came to the home, but Pat was told there wasn’t anything illegal about storing flammables in a bedroom closet, as it was his home. The police had been to the home many times and were expressed concern about Matt’s mental condition, but told Pat there was nothing they could do but to “call if you have any more trouble”.
Pat confronted Matt when he came home from his walk with the dog. He became angry and threw a portable phone at his father. The police were called again and this time they took Matt to a hospital emergency room where he was placed under a psychiatric hold (PEC) because of his behavior.
Pat wanted doctors to realize how sick his son was so he began collecting evidence that his son was a danger to himself or others. Pat met with a family psychiatrist, and he wrote a letter stating that Pat was a credible parent and shouldn’t be dismissed as an alarmist. In the doctor’s “Matt needed long term care.” Pat also collected affidavits from Matt’s friends. One stated that Matt had shown him a “noose” that he had put around his neck. “This is how I am going to kill myself,” Matt was quoted as saying. Pat also took photos of the flammable explosive items in his son’s bedroom closet and hand-delivered them, along with a the family psychiatrist’s letter and the affidavits from Matt’s friends, to the hospital. He did this the very next day while his son was still being evaluated at the hospital. Pat even had the Jefferson Parish Coroners office involved to get their input to prevent an early discharge, and they agreed Matt should be kept past the 72 hour hold.
“No one paid any attention to them or to me,” Pat says. “They told me that HIPAA kept them from telling me anything about my son.”
Undeterred, Pat called the hospital official in charge of patient care and begged her to arrange a meeting for them with Matt’s doctors. “She replied HIPAA, HIPAA. I told her in no uncertain terms that ‘I did not need to discuss Matt’s medical condition, I know that!’ I told her I wanted to discuss with the doctors — any doctor — what we should be doing at home to help Matt when he was released, how to save our son.” Pat was told he would get a call back but never did.
At that point, Pat contacted his local congressional representative to learn about HIPAA. He wanted to learn more about it’s restrictions and also wanted to make certain that he understood the ramifications of a PEC’s Psych patients rights as per HIPAA. The Congressman’s legal rep told them it was “unclear” as to whether or not the doctors could talk to Pat and Debbie since Matt had been committed.In short, not even the congressman understood the HIPAA law.
Pat next sent a fax to the hospital’s CEO begging him to have someone talk to Pat and Debbie before Matt was discharged. Pat never got a response from the CEO’s office.
While Pat was trying to tell hospital officials that his son was sick and going to kill himself, Matt was denying that he had a mental problem. According to the medical records, Matt insisted his parents were overreacting. When asked about the contents in his closet, Matt said that he understood why his parents were worried but he insisted that he wasn’t going to harm himself. He also told the doctors that he “didn’t believe mental illnesses were real”.
On Oct. 8th, the medical team evaluating Matt noted in his chart that his judgment was “poor.” Despite this, doctors began planning discharge procedures. Pat was furious. “He wasn’t ready.” In total, Matt had been in the hospital five days. “The doctor’s told me that my son had promised to take his medication, as they had developed a “delicate bond with him”….. and there were no signs that Matt was dangerous or suicidal. I said, ‘Bullshit. My son won’t take his meds…He will kill himself!”
Pat told them his son was still paranoid and having hallucinations in the Psych unit. “One of Matt’s friends had visited him two days before and Matt had complained FBI agents wearing invisible raincoats walking inside the hospital.” The doctors said they had not noticed that.
When Pat realized that no one was listening and that his son was going to be discharged, one way or the other, he asked the doctors to give his son a long-acting , injectable anti-psychotic drug that would keep him stable for at least thirty days. The doctors said they asked Matt but he refused. However, Matt did agree to outpatient treatment.
Matt’s discharge plan called for him to attend a local treatment program. But when his mother drove him to the center, he balked, saying he was scared that the people inside were going to harm him and it was a “trap.” She coaxed him into the center but was told by the staff there that they couldn’t discuss anything about Matt’s treatment or if he participated in therapy. “HIPAA again. At home, he refused to take his medications, and the meds he had taken at the hospital were wearing off as was expected.” Pat recalls.
Eight days after Matt was discharged, he offered to cook his father breakfast. After he fixed scrambled eggs, he announced that he was going upstairs to get ready for his out-patient therapy class. Before leaving the kitchen, Pat gave Matt a hug and told him “I love you”.
Inside his bedroom, Matt opened the valves on the propane tanks, took the caps off the gas cans and fired a home made shotgun shell device killing himself. His father raced upstairs and found him dead. Pat tried CPR to no avail.
Pat believes the doctor who discharged him “hoped” Matt was stable. But Pat thinks “this had more to do with insurance money than my son’s health.” Even though Matt was in the Psych unit in the same hospital in the same building as his primary long term psychiatric doctor, the medical records do not show Matt’s primary doctor was ever consulted. Why? Pat asks. The records are unclear to whether or not the Coroner’s office played a role in Matt’s discharge.
Pat remembers being told at the hospital discharge meeting, “Your son is stable—we need to release him, the insurance company will pay for one more day.” Pat says, “The doctors and insurance company said they ‘knew better’ than us. They refused to listen to us and our repeated warnings. It was all about money. We were his parents. We loved him and wanted to protect him. But he was released to society, ready to kill or be kiIled and there was nothing we could do to stop it.”
Pat still wonders “what more could we have done. What more can a parent do?” He is still searching for answers and he will “till my dying day. I want to do what I can to keep this from happening to other parents. That’s why I’m sharing my story. Our politicians need to educate themselves about mental illnesses and we need to change our laws through the legislature and change medical protocals. No other families should lose their son, like we have.”




This could be the saddest story ever. What has happened to our healthcare system that common sense and compassion have completely gone out the window? These parents must be raging. I’m raging. And with the tsunami of dementia rolling in, (50% > 85) many who live alone…I’m not sure they/we have a prayer.
This story conjures up so many emotions. I am angry at the system, I am heartbroken for Matt and for his family, and I am TERRIFIED that a variant of this could be our family’s story. I consider myself to be a fairly savvy consumer when it comes to mental healthcare; we’ve been living with it in our family for 13 years. Thankfully we have insurance, an advance directive for our 20 year old, a strong support network and reasonable resources to help our children. However, even that is not enough.
Our younger daughter’s latest relapse of her illness has brought us to one brick wall after another. At 16, she has the right to deny treatment, to check herself out of any hospital or treatment program. Our options include getting a court order for inpatient treatment, but that can take up to 60 days, and we will have no say as to where our daughter is placed. Or, if she shows signs of being a threat to herself or others, we can call the police and maybe they will handcuff her and place her in a 72 hour hold. But then, we’re back to square one. Even though we know that she is self injurious, no one can look at her injuries unless she gives permission.
In less than 2 years, we will have virtually NO ability to keep our daughter safe.The reality is that when she needs help the most, when she is most at risk for harm, her view of the world and the people in it is very distorted. We become the enemy, ones not to be trusted, and the more we try, the more we offer our love, our concern, our support, the more the door is slammed in our faces. And the system seems to be in handcuffs and shackles, unable to do what is truly best, what is truly necessary to save lives.
I wish I had some answers, I am generally someone who is solution focused, who believes that there is always a way. But in the past month it feels like I have shed enough tears of frustration, heartbreak and sheer helplessness to end a drought.
At the risk of sounding completely bitter, I can’t help but think that if the outcome had been different for Matt, if he had turned the gun away from himself rather than towards himself, more people would sit up and take notice, and demand that something change. How backwards is that?
HIPPA was a problem when my daughter was hospitalized and I think it should be changed to allow better exchange of information with families. However, in this tragic story you mentioned, it appears that both the doctors and parents were aware that treatment was definitely required. What needs to change is requiring insurance companies to pay for longer stays in a hospital, for more hospital beds to be available (too many state hospitals have been closed around the country), and for more effective inpatient and outpatient treatment laws. Consistent treatment over a sustained period of time is often required for someone with a severe mental illness and, unfortunately, if the person lacks insight to remain in treatment after being discharged from a hospital, the treatment ends and a revolving door of hospitalizations begins. A mental health system, governed by sensible treatment laws, would provide sustained, consistent treatment that would put someone with severe mental illness on the road to recovery.
Pete, thanks for the chance to sound off on H IP PA. After watching the Senate hearing, at which you gave testimony, it is clear to me that our privacy law is not being used the way it is intended.
I have always been able to get basic information starting with my sons diagnosis at the age of 21. The doctor took me in a corner, and in a hushed tone said,”I am not supposed to share this information with you, but I believe your son is bipolar. I would suggest that you take him from this crisis center home or to a hospital.”
What hospital???? Well this was all new to me. It was clear that my son had totally lost touch with reality. I did what the doctor told me to. I took him home. I filled the two week prescription. I gave him the medication and watched him fall asleep. Grateful for the respite, but I have never been to a darker lonelier place in my whole life. His bizarre behaviour resumed when he woke up. I took him to a hospital. They wouldn’t keep him. I took him to another hospital. They would not admit him either. So the doctor who thought she was helping by sending him home with me gave me no resources to cope. Thank goodness for NAMI. NAMI isn’t enough but it was all i had. But for the record the doctor didn’t tell me about NAMI.
HIPPA states that the doctor may share information if it is in the best interest of the patient. The doctor believing that it was in the patient’s best interest to tell me my son’s diagnosis and send them home with me did so secretly. Why? is she misinformed amour HIPPA? is there a double standard here. If it is in the best interest of the patient to send them home with the family, surely it is in the best interest of the patient to inform the family about basic patient needs. We do this with other illnesses.
Not enough hospital beds means a doctor has to make tough choices. Is this what motivated the doctor to send my son home with me? Did she think of here’s a reasonable family–he’ll be safe. In our state, we have 11.4 beds per 100,000 people. The recommended number is 50. The poor doctor needs to put four people in one bed. Not enough beds means not enough nurses, social workers, peer support, and doctors to treat the people with severe mental illness or help the families. Unfortunately, I’ve had conversations with treatment providers that sound like an apology. “I wish I could do something, but if he’s not homeless there’s really nothing I can do.” or “I wish I could keep him, but if he’s not saying he’s homicidal or suicidal I can’t keep him.” Yes, I have had absurd conversations with treatment providers. Lack of resources means lack of options. It is sad commentary that keeps us focused on helping individuals in crisis. Now that i know better, the last time he had a break, he was admitted for 4 days. But i am left feeling, what is the point? A temporary band-aid on a chronic problem.Our goal needs to be to avoid crises. If we could integrate individuals so that they are protected within our communities, our families could get some peace. HIPPA is a symptom of our don’t ask, don’t treat system.
From the story above it appears the patient signed a release for his parents, but the mental health professionals ignored it. The problem in this story wasn’t HIPAA. Wonder why the mental health professionals didn’t follow the wishes of the patient to release information to his parents? Also, it doesn’t sound like the mental health professionals did much with the information the parents provided to them, so not sure what HIPAA has to do with that either.
Hippa is one crazy set of stipulatios probably invented by Mental Health Hygeine lawyers and civil libertarians. It serves no-one, and certainly not the mentally ill. When a person is treated for a psychosis that puts him/herself or others at risk, and is clearly. diagnosably in a state of insanity, there should be no Hippa constraints. Every and all people including treatment team, doctors, and involved family should have all information about the patient that they need to help him/her. This is common sense! No one heals in a vacuum. The mentally ill need a well-informed environment to assist them to recover. To withold useful info from the direct caregivers, often the family, is like refusing to treat a cut w/ neosporin, or like pulling someone half way out of a burning building.
Is it a ruse?? Hey – the less informed a loving family is, the less chance for their mentally ill one to recover with their real help. – More money for the corrupt mental health system. Hope I’m wrong.
Hippa is fine for those who are still in their right mind, and want a little touch-up mental health work. For the most serious mentally ill, Hippa ensures that when they return to family, the family will have little to go on, to help them. Hippa locks the seriously mentally ill into illness. With knowledge is power – with full knowledge into a loved one’s illness, there is the power to bring about healing. Hippa also reinforces stigma – as the patient becomes convinced that his/her mental condition is something to hide.
There needs to be a class action lawsuit against the entire Hippa system. Those who implemented and uphold the Hippa standards are guilty of much wrongdoing, as witholding patient info from those most likely to love and help them, does the mentally ill much harm, even to death.
This is happening all across the country and another example of our broken, “no one cares” medical system. Any wonder that we have mass murders committed by folks clearly in need of help but parents that are powerless to get them help. Society as a whole pays. And rather than fix this our congress is advocating more gun controls, like that is going to stop mass murders. Boston marathon killings didn’t involve guns.
Even with a “signed” release they do not release the information. My brother signed a release, although I got a tid bit more of information than this family did, it did no good. I had to drag it out of them!
As with this family the treating professionals did not head my warning them, “he is going to kill himself” “he is trying to kill himself””please help me”
I agree with Pat, it’s all about the Money! It’s not HIPPA that keeps information from us, it’s the treating professioanls! They also lie to us on a constant basis. Why is that? These treating prfessionals do not believe what the family tells them either. Why is that?
This issue-mental dysfunction. Is a gold mine, they don’t give a hoot about our loved ones