A front page story in The Washington Post yesterday was published under the headline: “Hinckley: Man on the mend or a danger?”
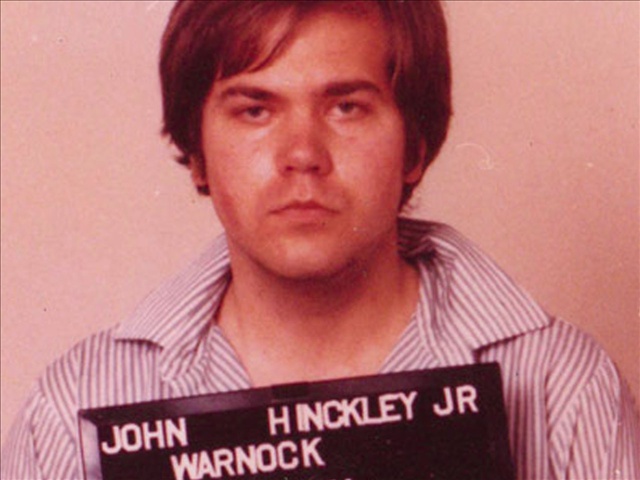
According to the story, a federal judge will decide the fate of would-be assasin John W. Hinckley Jr., this week after listening to five days of testimony. Hinckley’s family members, as well as his doctors and case manager, claim the now 56-year old Hinckley does not present a danger either to himself or to the community. The depression and unspecified mental disorder that drove him — along with his narcissistic personality disorder — to nearly kill President Ronald Reagan in 1981 are now all under control.
That’s not so, prosecutors claim. They insist that Hinckley, who has spent the past three decades in mental facilities, is deceptive, lazy, and can’t be trusted. The Post quoted Assistant U.S. Attorney Sarah Chasson stating, “Mr. Hinckley has not been a good risk in the past and, therefore, is not going to be a good risk in the future.”
The judge is being asked to determine if Hinckley is “dangerous.” If he is, the judge will not grant him more freedom than the ten day visits that he currently is allowed periodically with his mother — while being monitored by the U.S. Secret Service.
I often am asked how “dangerous” became the criteria that is used to decide if someone is so mentally ill that he/she can be involuntarily held and forced to undergo treatment. The question is an important one, especially for those of us who have loved ones with mental disorders.
If you read my book, CRAZY, you know that I tried to get my son help when he suffered a psychotic break, only to be turned away by an emergency room doctor who said my son didn’t meet Virginia’s “imminent danger” criteria. Some forty-eight hours later, my son was arrested after he broke into a stranger’s house to take a bubble bath.
The dangerous standard has become so widely accepted in the U.S. that it has become the de facto criteria that many insurance companies now use in deciding if someone who wants to voluntarily enter a treatment program will have their mental health care costs covered.
Most scholars credit the Lanterman-Petris-Short Act, which was approved by the California legislature in 1967, as the beginning of a civil rights movement in mental health law. But while the LPS, as it is known, opened the door, it was Lessard v Schmidt – a Wisconsin civil case in 1971 — that radically changed mental health laws.
After purportedly trying to kill herself, Alberta Lessard was involuntarily committed to a state facility where she was diagnosed as suffering from paranoid schizophrenia. She enlisted help from local civil rights activists who filed a class action lawsuit challenging the Wisconsin’s civil commitment law. As was common at the time, involuntary commitment laws were unclear and broad. In Wisconsin, a “mentally ill individual” could be involuntarily committed if “he required care and treatment for his own welfare or the welfare of others or of the community.”
Lessard’s attorneys successfully argued that if the state intended to deprive an individual of his/her freedom in a civil commitment hearing, then that citizen deserved the same legal protections as an accused criminal whose freedom also was at risk. The judge agreed and, among other things, ruled that persons with mental illnesses had a right to a jury trial, the right to appointed counsel, the right to remain silent, exclusion of hearsay evidence and proof beyond a reasonable doubt. In short, the Lessard decision caused a major swing in the pendulum.
The Lessard case also established that immediate dangerousness had to be shown. There had to be evidence of “an extreme likelihood that if the person is not confined he will do immediate harm to himself or others” otherwise, there could be no forced commitment. It was a popular concept born from the 1960s. If someone is not hurting himself or anyone else, then why interfere?
The Lessard decision made its way to the U.S. Supreme Court, which sent it back to lower courts twice for revisions. In one ruling, the word “extreme” was replaced with “imminent danger.” Eventually, the Wisconsin legislature reacted to the Lessard case by drafting a new civil commitment law that required imminent physical dangerous to self or others (homicidal or suicidal.) Other states soon began patterning their laws after Lessard and “imminent dangerousness” became the test.
It soon became obvious that the “imminent dangerous” criteria was itself, dangerous. In one well publicized court case, a man who had a long history of schizophrenia who was sleeping under cars at night and eating his own feces was not considered to be a danger to himself or others because neither of those acts was proven to be harmful to his health.
Dr. Darold Treffert, a Wisconsin doctor and veteran mental health leader in the state, was among the first to document tragedies where clearly psychotic individuals died because they were not considered dangerous and could not be forced into a hospital, but were so psychotic that they literally froze to death in the streets during harsh winters, committed suicide or died because of circumstances clearly tied to their untreated illnesses. Dr. Treffert coined the term “dying with their rights on.”
By 1995, thirty-five states and the District of Columbia had amended their civil commitment laws. Most dropped “imminent” and simply said a person had to be “dangerous.” Others decided that judges could consider other criteria such as “gravely disabled” or “unable to care for self or others.”
Ironically, Wisconsin went even further in 1996 when its legislature modified its civil commitment laws. The new language allows commitment if there appears to be a “substantial probability” that the ill person “needs care and treatment to prevent further disability or deterioration” and ” if left untreated… [will] suffer severe mental, emotional or physical harm…” and “[shows] an incapability of expressing an understanding of the advantages and disadvantages of accepting medication or treatment, and, of the alternatives to the particular medication or treatment offered, after the advantages/disadvantages and alternatives have been explained.”
Talk about a swinging pendulum. The new law is certainly much different from what the Wisconsin legislature unleashed after Lessard.
The problem with using “dangerousness” should be obvious. A friend of mine was bringing her adult son home from his appointment with his psychiatrist in New York when they ran into a traffic jam on the Verrazano bridge. The doctor had just assured my friend that her son was stable. Without saying a word, the young man opened the car door and leaped to his death.
Ironically, in the same Sunday edition of The Washington Post, there was another story that caught my eye. It was about Thursday’s fatal shooting of a campus police officer on the Virginia Tech campus in Blacksburg. The 22 year old shooter, who committed suicide after murdering the officer, was from a nearby town and had no known history of mental illness or known drug problems, the article reported. In fact, his friends saw nothing that would suggest he was dangerous.
Obviously, the judge in the Hinckley case is being asked to decide if it is safe to allow Hinckley more freedom. He is not being asked to decide if an “imminent danger” exists that justifies Hinckley being involuntarily held. That issue became mute as soon as Hinckley shot the president. Just the same, I am curious about how the judge will make his decision.
According to the Post, prosecutors will claim that Hinckley continues to be dangerous because since the 1981 shooting, he has:
1. had failed relationships with three women, all of whom, he met while they were patients with him in a mental hospital. In one instance, he invited two of them to the same party at the hospital at the same time.
2. that he lied twice about going to see movies, when he actually went into bookstores. On one occasion, he was seen scanning books about President Reagan, including one that described the attempted assassination.
3. that he looked up photos of a dentist on the Internet and then faked a tooth ache so he could meet her.
His therapists claim the three flaws cited above were simply examples of his “poor judgment.” The prosecutor sees something more sinister. I suspect the judge will not know — even after listening to testimony for five days — if Hinckley continues to be a threat. I suspect the judge will make his decision based on community safety or what’s politically expedient.
What I do know is this. If Hinckley had not fired at the president, were free today, and his family was concerned about his actions and asked a court to involuntarily commit him based on the three flaws cited above, he would not meet the “dangerousness” criteria and his parents would be unable to force him into treatment.
Which brings me to the point of this blog. Predicting dangerousness is fraught with error. It is a foolish criteria.
How interesting then, that we have laws that prevent concerned parents and doctors from intervening when an adult is clearly psychotic (sleeping under cars and eating feces) until that individual becomes dangerous — and then once that person crosses that line, we decide that the slightest oddity in their behavior — such as inviting two women to a party at the same time — is an ominious signal that the person is untrustworthy.




Thanks so much Pete for yor hard work. I so appreciate it.
I have heard complaints about the “dangerousness” criteria from many — including, of course, you — and, though I can understand the concern, I have not read someone propose a Constitutional and fair alternative. You cannot, and should not be able, to hospitalize someone involuntarily simply because they have a diagnosis of mental illness (or are currently suffering from one). That is absurd – and the reasons should, but do not seem to be, obvious.
Every law in this country is a balancing act. It is a balancing act between the rights of the individual, the rights of others and a society’s need to preserve functioning. In this instance, a person has a right to their freedom; other people have a right to the same; and society would cease to function if violence were rampant and/or ignored. We involuntarily hospitalize people, for the most part, to protect the safety of others (their rights) and, to a lesser extent, to preserve functioning; some may argue that, by preserving the life of an individual, you are also protecting their right (life).
Of course, for many suffering from mental illness, being in the hospital, health wise, would be better. Very few argue that these cases do not exist. The question, then, from a legal standpoint, is if that fact alone is enough to strip someone of their rights. Here is the problem with it: nowhere in the above, nowhere in the Constitution, nowhere in any Supreme Court document will you find something that says “one can deprive someone of their rights because it is (arguably) better for them.” Nowhere. And the courts do not exist to ensure the health of American citizens. They exist to protect the rights of American citizens, to uphold that balance and to uphold the Constitution. If one were to allow involuntary commitment on the sole bases of the diagnosis of a mental illness, or even of loss of insight, the Courts no longer are doing that. And that balance is no longer kept in balance — it is tipped too far away from protecting the rights of the individual.
Note that I said *rights*, not necessarily *best interest*. There is a difference.
I am not saying that the dangerousness criteria is perfect; however, I am saying that you have to put something better on the table if you want something to change. In the case of the man who leaped from the car, what would you have suggested be done? If he was ruled stable, there was nothing at all that would have predicted his actions. I do think using that anecdote is telling. As people, the feeling that I believe that we hate, more than anything, is powerlessness; a lack of control. Even if there was nothing that could have been done and nothing that could be done, we often feel compelled to do SOMETHING, even if that something does not fix the problem or would be a negative (taking away rights), more than a positive. When arguing for a side, think carefully to make sure your arguments are not guided by these emotions.
One potential solution is to more clearly define dangerousness — in a way that still allows for balance — as it is clear to see that it is currently subject to quite a bit subjectivity. Depending on the definition, I may be more open to reconsider. A strong public outpatient system (NOT AOT) is also called for. You can involuntarily commit someone all you want; in most situations, you still have to send them home.
Having seperate standards for treatment for people with mental illness versus other medical disorders is to me discrimination. The fair and equitable way to determine need for treatment is whether the person has the capacity to recognize they have an illness, weigh the benefits and detriments of that treatment as well as the consequences of their choice. That is the standard that is used for other medical conditions. That is the standard that should be used for mental illness. Current standards that only rely on danger are civilly and morally wrong and irresponsible.
Interesting argument and one that I have seen stated before. I will respond in two parts:
(1) The dangerousness criteria — The dangerous criteria is one that I can understand, as it involves protecting the rights of others and maintaining functioning. As a society, we intervene when someone is dangerous all the time. The primary difference between those with mental illness and those without is that, when a person is found to be dangerous due to mental illness, they are involuntarily committed; for someone who is not mentally ill, they are charged with “Conspiracy to Commit _____.” If the person with mental illness were to be treated equally, that would be the route they would have to take, as well.
One could, of course, argue that this is how it should be. I’m not apt to automatically disagree, as I feel that viewpoint has some validity to it. The question then, of course, would be if it tips the scale too far away from protecting the rights of others.
Perhaps there is also a middle ground. Someone suffering from an Infectious Disease can be ordered into isolation in extreme cases (danger to others). The law could be revised to further clarify what “extreme” means. If this were the case, though, the dangerousness criteria would only become more exclusive. Once again, we must examine what that does to the balance and how it fits in context on the Constitution.
Danger to self is another issue and one that lies much deeper. In this country, nobody, no matter their physical or mental state (with the exception of a few states who allow it in cases of terminal illness), has a right to kill themselves. The question here would be: Does someone of sound mind have a right to take their life?
(2) The issue with changing commitment standards to reflect one’s capacity to understand their illness is that, when discussing this, I have noticed that many impose different standards on the mentally ill than on the physically ill. As an example, many believe that a young man suffering from psychosis who believes he does not need medication — but is not a danger to himself — would fall under this category. In this case, one could argue that his behavior shows that he does not understand the true nature of his illness. But what about the Diabetic who believes that medication is burdensome and that he/she can get by without it? Clearly, this patient does not understand the true nature of his illness. To be truly non-discriminatory, then, we would have to involuntarily commit both of them to treatment. Most mental health “advocates” I have talked to, however, would not.
And, of course, when you change the criteria, you must once again consult that balance and the Constitution.
Furthermore, as you actually seemed to be alluding to one’s competency to make medical decisions in your original post, it is important to understand what that means. From Standford Law (h tt p : // www . stanford . edu / group / psylawseminar /Competency . htm) (short version quoted — see actual mandate in full):
“Legally, a patient is incompetent if unable to do the following: (1) respond
knowingly and intelligently to questions about recommended treatment; (2)
participate in treatment decisions by means of rational thought processes;
and (3) understand the items of minimum basic medical treatment information
with respect to that treatment.”
In light of this, let us look at hypothetical Patient John Doe. John Doe is suffering from a psychotic break and his parents want him involuntarily committed (either outpatient or inpatient). He refuses to take medication as the side effects are, in his opinion, intolerable; he also doesn’t feel much better on them, by his own experience. His parents feel differently, noticing a drastic difference in his behavior on/off medication — namely that, on medication, he does not converse with hallucinations and pace his room endlessly. John does not feel he actually is psychotic and, instead, his life is disrupted by religious experience best treated by the clergy.
Is John incompetent to make medical decisions?
(1) John knows quite a bit about the treatment recommended to him. He knows they are being given to stop the voices (or, to him, his “spirit guides”), he knows they are prescribed for hallucinations (but he does not feel he has them) and he knows their side effects. It is likely he can do what is required in (1).
(2) “Rational thought processes” — what a gray area! He is delusional in a clinical sense; however, he is able to clearly articulate that he does not wish to take medication as they cause unpleasant side effects and he views his experiences to be supernatural ones, not those that are a part of disease process. It is possible he will be ruled able to meet the standards set in (2). It is possible that he would not, depending on the consulting professional.
(3) As listed in the expanded version, this includes “(A) The nature and seriousness of the illness, disorder, or defect
that the person has.” This is where one would seem to have the strongest case against John’s competency; however, the patient must be unable to do ALL of the following. If he can meet (1) and (2), then he is no more incompetent than the diabetic. In addition, one (aka, a lawyer) could argue that he understands there is a significant disruption in life, he just has differing views on the cause. Do we involuntarily commit everyone sitting in the pews on Sunday?
Pete, just to re-iterate a main and important point here:
The issue of involuntarily commitment is, ultimately, not a medical one, which would be answered by asking “What is in the patient’s best medical interest?” It is a legal one. Nor can it ever be a medical issue, as it involves taking away a legal right. That is important to remember as, if you want the requirement to change, you MUST make a legal argument, not “it would improve his/her health”.
Pete,
On the same day that your wrote your blog, the Milwaukee newspaper published a long story about the dangerous criteria and Alberta Lessard. It is well worth reading. Unfortunately, because you limit the length of comments, I have to send it in two pieces. Notice that more than 80 people have commented on the story at the newspaper’s website.
Law creates barriers to getting care for mentally ill
By Meg Kissinger of the Journal Sentinel
Dec. 10, 2011 |(80) CommentsMartha Wilson trudged up the hill, sick with worry, arms pumping, head down, too distracted to notice the brilliant April sun rising over Lake Michigan. It was Richard.Her son wasn’t taking his medicine. He didn’t like how it made him feel thick-headed and spacey.At first, Martha and her husband, Jeff, thought their son’s brooding and his drastic mood swings were just typical teenage angst. All teenagers lash out from time to time.Then Richard started mumbling, talking about curses and bizarre plots. He thought his grandfather’s real estate business was a front for a drug operation and that his family was under some kind of spell dating back 127 years. He heard voices.Stop him. Stop him.After Richard threatened his parents with a knife in November 2010, they got him to a psychiatrist, who diagnosed Richard with schizophrenia.The medicine seemed to help with the delusions, but Richard began to balk. Martha wished they could force him to take it. To do so, they would have to go to court and prove he was a danger to himself or others. It would be awful to drag him through that, a kind of betrayal.When Richard was little and had an infection, Martha could get him to take the antibiotics that tasted like pink bubble gum without any problem. Now he was 17 years old. He weighed 160 pounds.That was no match.There are 4 million people in the United States with severe mental illness. Only about 40,000, or 1%, are dangerous. Even then, the violence is usually minor – a punch or a shove, said Jeffrey Swanson, a Duke University professor who has studied the correlation between mental illness and violence for more than 20 years.People with mental illness are 13 times more likely to be a victim of a crime than the perpetrator. Still, the inability to identify who is dangerous and the barriers to getting them care are among the more wrenching failures of our time.April 14, 2007: Virginia Tech University, Blacksburg, Va. A professor walking across campus noticed something curious – a man practicing locking the front door of Norris Hall with chains.Two days later, Seung-Hui Cho, a senior, chained that same door shut and scrambled up to the second floor, where he sprayed four classrooms with bullets before shooting himself in the head. Thirty-three died and 25 were injured. It was the deadliest school shooting in American history.Cho, 23, had been under a court order to get psychiatric treatment for severe anxiety disorder. No one bothered to make sure he followed through.June 1, 2010: Tucson, Ariz. Lynda Sorenson, 52, sent an email to a friend about how frightened she was of Jared Loughner, a 22-year-old fellow student in her basic algebra class at Pima Community College.”We have a mentally unstable person in the class that scares the living crap out of me,” she wrote. “He is one of those whose picture you see on the news after he has come in to class with an automatic weapon.”On Jan. 8, 2011, seven months after Sorenson’s nervous message, Loughner walked up to U.S. Rep. Gabrielle Giffords at a Tucson shopping center and shot the congresswoman in the head. He turned to the crowd, killing six people, including a federal judge, Gifford’s aide and a precocious 9-year-old girl who had gone with her neighbor to the “Congress on Your Corner” event for a chance to meet the lawmaker. Twelve others, besides Giffords, were wounded.On that day alone, there were at least two opportunities to stop Loughner. An officer with the Arizona Game and Fish Department pulled him over for running a red light, but found nothing suspicious and let him go. When Loughner arrived home, his father tried to grab the bag his son was carrying, but Loughner wrested it away and ran toward the desert.***If a man standing in a crowd clutches his chest and collapses, people will rush to help. But if that man has schizophrenia and mumbles or cries uncontrollably, chances are he’ll be ignored.”People are scared of mental illness,” said Jon Lehrmann, head of the psychiatry department at the Medical College of Wisconsin. “The natural tendency is to look the other way.”Nor is there an expectation that we should help, as with illnesses that affect other parts of the body.”You never hear about people being held accountable under the Good Samaritan laws for turning away from someone in psychiatric crisis,” Lehrmann said.In fact, people often are discouraged from helping others get psychiatric help, as though they are being rude or meddling to suggest a psychological problem, Lehrmann said. Mental illness is shrouded in shame and secrecy in ways other illnesses are not.Why didn’t people around Cho or Loughner do more to make sure these obviously ill men got care and that others around them were safe? Why couldn’t Martha and Jeff Wilson force their troubled son to take the medicine that might make him well?The answer begins 40 years ago on the second-story window sill of Alberta Lessard’s West Allis apartment.***Alberta Lessard could hear their footsteps, smell their cigarettes. Goons trained by Richard Nixon were coming to kill her.She threw open the window and climbed onto the ledge. It was a Friday afternoon, Oct. 29, 1971.A neighbor called the police. Assuming she was trying to kill herself, the two officers yanked Lessard inside, handcuffed her and hauled her back to the county mental hospital.Lessard was becoming a regular at the asylum, one of the largest of its kind in the country. She had been committed three times in the previous two years. Doctors who examined her said she had schizophrenia with paranoid delusions.Milwaukee County’s Asylum for the Chronic Insane, as it had been called, was a Cream City brick building, a Victorian-era behemoth, sitting atop a hill like something out of a Frankenstein movie. There were spires, a winding staircase and thick metal doors that clicked shut. The long corridors smelled of urine and chlorine.It was not a place of healing, as far as Lessard could see.Attendants held the patients down with leather straps and injected them with sedatives. The drugs made their arms and legs stiff and their thinking cloudy. They drooled.One of her dormitory roommates screamed until she vomited, then licked the vomit off the floor and started screaming again.It wasn’t hard for police to put Lessard back inside. All that was required to commit a person to a mental hospital was an affidavit signed by three people saying the patient was sick and in need of treatment.”It was easy,” said Laurence Kauth, a psychiatrist at the mental hospital in that era. “Too easy.”Around the nation, psychiatric wards were full of people no one wanted to care for.”I had a woman once who tried to commit her mother because she was going out of town on vacation and wanted us to watch her,” Kauth said.Lessard, then 51, had been fired from her job as a West Allis schoolteacher for refusing to use a new reading curriculum that she considered “garbage.” She also had been fired from Marquette University, where she was working on her doctoral degree and was teaching reading specialists. She began to call the office, sometimes 100 or more times a day.The daughter of a lumberjack and midwife from northern Wisconsin would not be “put away” without a fight.Her persistence would change mental health care across America. She would pave the way to ending easy involuntary commitment for hundreds of thousands of people who were able to take care of themselves.Lessard wasn’t thinking of that on that October day. She was simply hiding from the goons.”They were coming to kill me,” Lessard said, recounting the story. “What was I supposed to do? Sit there and let it happen?”Whatever Lessard’s intentions were as she dangled from the ledge, a fall from her window likely wouldn’t have killed her.Her feet fluttered 18 inches above a riding snow blower parked in the lot of the hardware store that occupied the building’s first floor.***As she walked along the lake last April, Martha Wilson desperately searched her mind for something more they could do to keep Richard safe. Tony Meyer, a friend of Martha’s parents, is considered one of the premier adolescent psychiatrists in the country. At his suggestion, the Wilsons took all violent video games out of their Fox Point house. No one wanted to give Richard bad ideas.Jeff Wilson began working from home so he could be there when his son returned from school.Even after Richard pulled a knife on them, they couldn’t just put him in a locked psychiatric unit the way police had done with Lessard 40 years earlier. By state law, parents who want to commit their children 14 years old and older have to file a petition and get permission from a judge. They would have to prove that Richard was an immediate danger.One counselor after another told them the same thing: Unless he’s got a gun in his hands, he won’t meet the requirement.The Wilsons’ worries about Richard turned to panic once he stopped taking his medication. No amount of coaxing worked.If Richard had leukemia or was in a car accident, he might have had his own Caring Bridge site. Friends might have brought over casseroles and sent cards. Instead, they changed the subject when Martha wondered out loud what to do.He was getting sicker.***There are tests to confirm cancer cells and blood analysis to detect diabetes. There is no test to determine dangerous mental illness. “The best indication of future violence is a history of violence,” said Mike McBride, a longtime Milwaukee psychiatrist.Sometimes there is no warning at all. Mental illness often doesn’t appear until the teens or early 20s.Sam Hengel of Marinette was a lovable kid, even-keeled and well-liked. A Boy Scout.On Nov. 29, 2010, the 15-year-old returned from the bathroom to his Western Civilization class with the duffel bag he had hidden in his locker. The bag contained two semiautomatic handguns, 200 rounds of ammunition and a hunting knife.For the next six hours, Sam held the teacher and 23 students hostage. Some wept quietly. Others wrote letters to their parents apologizing for not having been better children. When police stormed the classroom, Sam turned the gun on himself.”He was a real happy boy,” said his mother, Anne.***Three days after Lessard was brought into the psychiatric hospital in October 1971, the West Allis police officers who arrested her appeared in court to argue that she needed to be kept there indefinitely. Lessard was not told about the hearing.She was assigned a lawyer, Daniel Noonan. He was not hired to defend her civil rights or challenge the county’s claims that Lessard was insane. Noonan was there as a guardian to give his opinion of what was best for her, similar to the protection that children get in divorce proceedings.George Currier, a doctor for the county, recommended that Lessard be committed permanently.The Milwaukee County judge, Christ T. Seraphim, ordered her held for 10 more days and later extended the commitment indefinitely.In 1971, people with mental illness were presumed by the law to be helpless and in need of protection. The state acted as a parent, a public policy dating back to the English law known as parens patriae, Latin for “parent of the nation.”The state could hold mental patients for five months without giving them a hearing. A typical hearing lasted less than five minutes, and more than 90% of the cases ended with same the result: commitment.Lessard had good reason to fight such a verdict. People judged to be mentally ill could not vote, marry, drive a car or own property.”It was more like a prison than a hospital,” said Thomas Zander, a lawyer and psychologist, now retired, who spent years fighting to expand the legal rights of mental patients.Determined to have her commitment overturned and to get out of the asylum, Lessard found a pay phone in the hallway and called Robert Blondis, the only lawyer whose telephone number she knew by heart.Twenty-eight years old and two years out of law school, Blondis worked at Milwaukee Legal Services. He had met Lessard several months earlier when she came looking for someone to represent her in a discrimination case she hoped to bring against Marquette and the West Allis School District.Though they had turned down Lessard because her case didn’t fit the agency’s mission, Blondis thought the involuntary commitment issue could be a winner.Milwaukee Legal Services was founded in 1964 as part of Lyndon Johnson’s War on Poverty, a program to provide legal representation in civil matters, such as divorce and landlord complaints, for people too poor to afford their own lawyers.Across the country, Legal Services lawyers were looking for ways to expand civil rights, filing federal lawsuits and working to rewrite laws like those that denied blacks the right to sit in the front of buses or women the right to own property.Blondis knew nothing about mental health law. He had never been to the county’s mental hospital until the day he went to see Lessard.The place immediately scared him. Beyond the decrepit facility, there were reasons aplenty to be afraid. Nationally and statewide, the death rate was 10 times higher inside asylums than out.Years later, excavators digging up the asylum graveyard found evidence that patients who died at the public mental hospital had been buried naked, two to a coffin, identified only by tags tied to their wrists.Hospital administrators could save money by buying shorter, less expensive caskets. So undertakers amputated the legs to fit the bodies inside.***When Blondis got back to his office, he looked up Wisconsin’s commitment laws, known as Chapter 51. He couldn’t believe what he read. “There were essentially no rights for people who had been committed,” he said. “No hearing. No notice. No jury trial. No burden of proof. It was amazing to me.”Blondis and his associate Tom Dixon, then 27, devised their strategy over late-night beers.Instead of challenging Lessard’s commitment on the grounds that she was not mentally ill, they would file a federal class-action suit on behalf of all committed people, claiming the law denied their civil rights.This was risky.Failure could mean that people like Lessard – disturbed but not really dangerous – would end up being stuck in that prison of a place for the rest of their lives.Though some of Legal Services’ senior lawyers were nervous about the strategy, Blondis and Dixon filed their claim in Milwaukee’s Federal Court on Nov. 12, 1971.Eleven months later, a three-judge panel issued its ruling. The judges overturned Wisconsin’s commitment laws as unconstitutional, setting aside hundreds of years of legal precedent.The judges found that the stigma of mental commitment was worse than a criminal conviction and, therefore, should be used in only the most extreme cases. Mental patients had to be given the same civil protections that criminals got.In order to lock up people against their will, the government would have to prove beyond a reasonable doubt that patients were immediately dangerous based on recent acts, attempts or threats to do substantial physical harm to themselves or others.County lawyers across the state had 90 days to review the 8,000 or more cases to make sure patients met the criteria or the “inmates,” as they were called, would go free.”It was chaos,” Blondis said.Eventually the case was affirmed on appeal and sent to the U.S. Supreme Court. Even before the court upheld the new commitment standards, making them the law of the land, Wisconsin and several other states had rewritten their mental health laws.Blondis and Dixon toasted their victory with champagne, but a calamity of unintended consequences soon followed.The standard of imminent danger set by Lessard’s case would prove to be a tragically inaccurate measure for who was mentally ill and in need of being kept safe. Thousands of people who were sick – but not obviously immediately dangerous – would be set free without proper care.In time, even Lessard would be denied protection she desperately sought.By correcting one outrage, her case had created others.***The problem with leaving it up to a person to decide if he or she wants psychiatric care is that not everyone with mental illness knows they have it. Recent studies say as many as half of all people with serious mental illness suffer from a condition known as anosognosia (Greek for “no disease knowledge”).The condition was first noticed a century ago in stroke patients, amputees and the blind. Because of a neurological disorder in the front of their brains, patients with anosognosia cannot appreciate that the affected body parts do not work properly.Amputees will swear their missing limbs are there. The blind claim they can see.Anosognosia is not a willful denial motivated by embarrassment or obstinacy.”It is an utter lack of insight,” said Xavier Amador, professor of clinical psychology at Columbia University.If a person can’t understand he is sick, why would he agree to treatment?***Some Milwaukee judges refused to accept the Lessard ruling after it came out, predicting “preposterous and barbarous results.” Darold Treffert, then superintendent at Winnebago Mental Health Institute, the state’s largest psychiatric hospital, complained to reporters at the time that the decision set a threshold for commitment that was much too high. Across Wisconsin and the country, stories started to surface about former mental patients who froze to death or were killed sleeping on the streets.”People are dying with their rights on,” Treffert said.Civil liberties activists like Zander, the Milwaukee lawyer, saw that as patronizing.People with mental illness are not children who need to be tended to, Zander said.”They have a right to live the way they want, eccentricities and all.”In court hearings, lawyers representing people who faced commitment demanded that the protections guaranteed by Lessard’s case be granted.Some got commitment petitions dismissed on technicalities.Lehrmann, the Medical College doctor, recalled a case of a woman who was, in his opinion, dangerously ill but was let go because the affidavit he signed had the initials “FMLH” on the top and did not spell out Froedtert Memorial Lutheran Hospital.The commitment process had become as adversarial as a murder trial.Laws written after the Lessard decision, meant to eliminate abuses of power, prohibit anyone but police officers from bringing a person in for commitment.What had been mainly a medical matter was now being decided by police officers and judges.Milwaukee County Court Commissioner Rosemary Thornton’s calendar began to fill up with mental patients demanding to be set free. It was her job to determine if someone met the new criteria for commitment and could be held for another two weeks until a judge could decide on long-term commitment.Thornton saw about 35 people each day. Most of them ended up agreeing to treatment in exchange for their freedom, but lawyers for the county had few ways to check if the patients held up their end of the bargain and stayed on their medication.The fewer than 10% who were held would likely be set free at the final hearing. Long-term commitments became almost obsolete. In the year before Lessard’s lawsuit, Milwaukee granted more than 1,200 commitment petitions. Last year, 74 were granted.Nearly everyone who appeared before Thornton in those days denied they had mental illness.”It was impossible to get most of these people to agree to treatment because they didn’t think they were mentally ill,” said Thornton, who spent 15 years as a commissioner.She saw all kinds of bizarre behavior:One man had chopped off his arm with a guillotine in his basement, hoping it would make him more sexually attractive, Thornton said.Three men cut off their penises. A woman stuck needles in her liver. One man wore a football helmet because he said he could not control the urge to throw himself to the ground, hoping to crack his skull open.Thornton said she understood how important it was for people to live their lives in the way they chose.”Here’s the big question: Are they making that choice with a sound mind?”At night, as she left the courtroom, she was often startled by what she saw. Garbage cans were filled with pill bottles. Without anyone accountable for their care, patients would toss their medicine away as they walked out the door.***The pace of emptying out public mental hospitals began in 1965, when Medicaid refused to pay for care in free-standing psychiatric facilities of more than 16 beds. It greatly accelerated after the Lessard decision. The number of public psychiatric beds in Milwaukee County shrank from 1,609 in 1971 to 262 today. Nationally, it dwindled from a high of 558,000 in 1955 to roughly 40,000 in 2006, the last year there was an accounting.Taking people out of psychiatric institutions would have marked an extraordinary leap in social progress, if only they would have been treated in community-based mental health centers, said Swanson, the Duke professor.”Instead, we now have a public system of mental health care that is fragmented and grossly underfunded,” he said. “In fact, only 12% of people with diagnosable psychiatric disorders receive minimally adequate treatment.”Given that many with severe mental illness are too sick to hold down jobs or sustain family relationships, thousands have been cast out with no good place to go.The National Institute of Mental Health estimates there are 3.6 million American adults with severe mental illness that is untreated. Of those, 200,000 are homeless and 319,000 are in jails or prisons.Before the Lessard decision, there were three times more people confined to mental hospitals than jails and prisons. Today, 20 times more people with mental illness are incarcerated than in a medical facility.***Lessard became something of a celebrity in the years immediately after her famous court case. Free to come and go as she pleased, she showed up at other people’s commitment hearings and spoke about the need for full civil rights for mental patients. Lessard was so adept at quoting the new laws that one of the county’s public defenders recommended her to the chancellor at the University of Wisconsin-Madison for an honorary law degree. Though she was not selected, Lessard occasionally spoke to college and law school classes.Not everyone was impressed. People sent her mail, blaming her for changes in the law that kept them from committing their suicidal sons or daughters.”They hate me,” Lessard said. “They accused me of killing their children.”She had no money and no hope of a job.Delusions persisted and intensified. Lessard was more convinced than ever that goons were out to assassinate her.She started to sleep under bushes and on county buses, jumping off whenever she thought she saw someone coming for her. Some nights, she’d try to catch a nap at a George Webb restaurant or the all-night Kinko’s copy store on S. 76th St. She ate garbage from alleys and contracted pneumonia.More than once, she slept in the trash bins behind the mental health complex in Wauwatosa.”You’d be amazed how clean they are,” Lessard said.In the mid-1990s – he can’t recall exactly when – Robert Blondis got a call from Lessard, his old client. Once again, she was calling from the county mental hospital and needed his help.This time, she wanted to get in.Out of money and exhausted from sleeping on the streets, Lessard thought she’d try and get a few days rest at the hospital. But the doctor there told her she didn’t seem dangerous enough. They refused to admit her.Lessard found herself on the other side of the same locked door.
Here is the rest of the story.
Mental health care is different today in almost every way than it was when Lessard was first locked up. Medications have improved vastly, making it easier for people with severe mental illness to work and maintain family relationships. There is more care in the community.A diagnosis of bipolar, depression or schizophrenia does not carry nearly the stigma it once did. Some athletes and movie stars talk openly about their battles with mental illness.Still, scientific data on the causes and cures of mental illness are so scarce that it is impossible to describe with certainty the best approach in dealing with people who are suspected to be dangerous because of their mental illness, said Swanson, the Duke University professor.”We do not possess the data to do this reliably,” he said.There is an entrenched debate over how to get patients who might be dangerous into care before something terrible happens.E. Fuller Torrey, a psychiatrist and brain researcher, founded the Treatment Advocacy Center in Arlington, Va., in 1998 to lobby for assisted outpatient treatment – a court order that compels patients to get treatment in the community or be held in a locked facility.All but six states have laws along this line. Wisconsin led the way in 1995 with its law, known as the “Fifth Standard,” which allows for those who previously were found to be incompetent to be more easily committed, though the law is unevenly applied.New York adopted something like this in 1999. There, it is known as “Kendra’s Law,” after Kendra Webdale, who was pushed to her death in front of a subway train by a man with schizophrenia.Torrey points to studies in 2005 and 2009 that show how expanded court-ordered outpatient treatment cuts down on hospital costs, homelessness, arrests and incarceration.”It works,” he said.But it doesn’t catch everyone. Eligible patients have to meet certain criteria, including a diagnosis of mental illness, a history of not complying with care and a record of being unlikely to function in the community without supervision.Neither Cho, the Virginia Tech shooter, nor Loughner, the Tucson gunman, fit those criteria.”We have more work to do,” said Torrey.This strategy has its detractors.Zander, the psychologist and civil liberties lawyer, believes compelling a person to undergo treatment is not effective. Anytime you give a doctor the authority to restrict the patient’s freedom, you tip the balance. Then a meaningful therapeutic relationship is impossible, he said.”It’s built on a lack of trust,” Zander said. “That’s the E. Fuller Torrey approach, and it doesn’t work. That’s the approach that we had for hundreds of years, before the Lessard decision.”A better way, said Zander, is a model that encourages alliances between a patient and doctor “so that when an individual feels alienated from society and starts to ruminate about things he might do to others, the doctor or caseworker knows about it and gets him help.”But Zander’s approach presumes that people who are sick will get care, and people like Cho and Loughner often do not.There will always be people who fall through the cracks, Zander said.Just as some people die of cancer, others die of mental illness.”We can’t save everyone,” he said.There are differences, though.People with dangerous minds sometimes take others with them.***These are some of the ways violence from people who are mentally ill can be measured:Ross Zimmerman was out for an early Saturday morning hike when he heard that Gabby Giffords, the congresswoman, had been shot. He immediately called his son Gabe, Gifford’s assistant, to find out what was going on.There was no answer.He tried again.And again.And again.For the next three hours, Zimmerman and his wife frantically searched Tucson emergency rooms.”We didn’t know until later that afternoon that Gabe had been dead for hours,” Zimmerman said. “His body was still lying there at the shopping center.”As Zimmerman sits in the conference room of Giffords’ Tucson office, looking out over an Arizona sunset, he is lost for an answer about what can be done so that another father doesn’t have to go through this agony.”Our mechanism for identifying people with mental illness is flawed,” Zimmerman said. “It’s a tricky problem.”Zimmerman is not shy about crying when he thinks about how much he misses his son, shot dead at 30, soon after giving his girlfriend an engagement ring.”I want to talk about him, even if it hurts,” Zimmerman said.Colin Goddard has a metal rod in his leg where bullets from Cho’s gun shattered his bone. He remembers lying in a pool of his own warm blood that morning at Virginia Tech as he dialed 911 on his cellphone.”I can still see the look in his eyes,” he said of Cho, who came into the classroom three times shooting.Goddard, now 27, lives in Washington, D.C., and lobbies for tighter gun control for people who have been found to be mentally ill.Most days, he is able to keep his emotions under control. But there are days when he wonders: What if he hadn’t been late to class that day and was sitting where he normally did, where nine students and his professor died?Each weekday morning, Jerzy Nowak climbs the same flight of stairs that his wife, Jocelyne Couture-Nowak, a French professor, did on the morning of Cho’s killing spree. His Norris Hall office is the same room where his wife died.It’s been remodeled now as the Center for Peace Studies and Violence Prevention. They chose that place as a way to symbolize triumph over violence.Nowak’s eyes tear up as his thinks about how his daughter, then 12, has had to grow up without her mother.For the first few years, Nowak felt certain it was important for him to be a witness to the grief that untreated mental illness produces. But now, nearly five years later, he’s not so sure how long he can tell the story.”It’s very draining,” he said.Lucinda Roy, a Virginia Tech professor who had urged Cho to get psychiatric help for months before the massacre, said the university had policies that forbid her from pursuing further action unless Cho agreed to treatment.”I wish we all had done more,” she said. “It haunts me every day.”Ron Barber, Giffords’ district director, was shot in the face and leg by Loughner. The bullet that went in his cheek exited the back of his neck. The shot to his thigh hit a main artery and, were it not for the actions of a nurse in attendance, he would have bled to death while the ambulances slowly made their way through the crowd.Barber is convinced that if people understood the symptoms of mental illness and the consequences of failing to identify people who are dangerous, they would be more inclined to help.”Ignorance and the lack of information are at the heart of this,” Barber said.He knows about stigma and misunderstanding. Barber worked in mental health care for more than 40 years, including a term as director of the Arizona Division of Developmental Disabilities.***Pat Spoerl understands Martha Wilson’s dilemma. Parents must have a place to send their children who become dangerous, said Spoerl, who has struggled for more than 35 years to find a place to keep her son safe.”They see this behavior and they are terrified, locking their bedroom doors, hoping that their child won’t kill them,” she said. “They see this behavior that’s so scary. They have to have a place to go, an emergency psychiatric place to commit them.”Spoerl’s son, John, 51, has schizophrenia. He cherishes his freedom and would hate to be stuck behind a locked door.”You can’t just take away someone’s free will,” he said. “What if it’s more fun to have mental illness than dangerous?”The two sat down recently to discuss the unavoidable tension of their different priorities. John teases Pat and she chuckles with affection at his jokes. But there is a gravity to their conversation.Pat says that being hostage to voices in your head that say terrible things and make you feel frightened doesn’t sound like freedom to her.”It sounds more like Hell.”Pat and her husband, Joe, first tried to have John committed in 1976. John, then 17, had attempted suicide several times. He talked about being a prophet and fantasized about hurting children. Joe found his son running naked in the woods behind their Wauwatosa house.Joe’s law school friend, George Rice, was a lawyer for the county in charge of mental commitments at the time, giving the Spoerls hope they could get John into the hospital for treatment.Instead, Rice told them there was nothing he could do.”John wasn’t dangerous enough,” Pat said.It made Pat Spoerl livid the way the system pitted families against their mentally ill children.”Who cares about your child more than you do?”She saw the sideways glances at the grocery store. She heard murmurs from others, even relatives, who wondered why she couldn’t control her boy.The Spoerls were desperate for advice on how to navigate a system that seemed more concerned about protecting their son’s civil rights than keeping him safe. They joined the National Alliance on Mental Illness, a support group for families that was founded in Madison after the Lessard decision.The Spoerls and other parents huddled in community halls and church basements to share stories about how their families were faring.John was assigned to a case manager who has dispensed his medication and distributed his Social Security disability check for the last 30 years. John takes his medication without complaint, but he also uses street drugs, marijuana and crack, which cause him problems.Though he has never been found to be dangerous enough to require a long-term hospital stay, John has spent several months in jail for various crimes such as theft and drug possession. He nearly drowned a few years ago after his medicine made him so thirsty he drank too much water from a jail toilet.His father died in 2005. Pat moved to a condominium a few miles from their old house.She sees John occasionally and talks to him often, but does not want to tell him where she lives. Pat worries that her son will come insisting that she give him money that he’ll then use to buy drugs.”The professionals in the mental health community have to be honest about the percent of people who are not recovering,” she said. “It’s nice to talk sweet talk about recovery. And I know that many people can recover quite well. But it isn’t everybody.”***The brain is not an Etch-A-Sketch that you can just shake clean. Diagnostic imaging shows damage to the brain echoing from one psychiatric trauma to another, said Robert Rawski, a Milwaukee psychiatrist who often examines patients for their ability to face criminal proceedings.”Each episode leaves them a little more diminished than the last,” Rawski said.And the risk to them – and others – grows.Torrey’s organization keeps a registry of violent crimes committed by and against people with severe mental illness – the “Preventable Tragedies Database.” It’s a synopsis of 5,512 horror stories collected since 1987.The litany includes people such as Tonia Kigas Porter of Bangor, Maine, who admitted starving her 5-year-old daughter to death, believing the little girl was evil; and David Harold Coffin of Snohomish, Wash., who stabbed his 60-year-old mother as she watched TV because he had a dream telling him to do so.Cho at Virginia Tech and Loughner in Tucson are listed. There are 124 cases from Wisconsin, though the list is missing at least one:Richard Wilson.***Martha Wilson awakened before dawn on May 8 to find Richard downstairs pacing and more restless than normal. She told him to go back to bed.Martha and her two sons had gone to her parents’ house on Beaver Lake in Hartland the night before. Ron and Mary Siepmann had just returned from Arizona, where they spent the winter.The rest of the family was due there in a few hours for brunch.This would be a bittersweet Mother’s Day for the family. Mary Siepmann was in the final stages of lung cancer.Martha Wilson had always depended on her family but never more so since Richard had been diagnosed with schizophrenia.When Martha was a scared, homesick freshman at the University of Wisconsin-Madison in 1979, her dad would send her funny cards to cheer her up, signed only “Your Secret Pal.”She taped each one to her wall. By the end of that year, the wall was covered with cards.Martha was busy getting her parents’ stuff unpacked. As the morning wore on, she became increasingly worried about Richard. Where was he?She found him just before 11 a.m. as her brother, his wife and their three young daughters were arriving. Richard was running down the road.That’s odd, Martha thought.Richard was sweating and out of breath. He said he’d been exercising.It wasn’t like Richard to go running.He was smiling.It’s a good day, he said.Have you seen your grandfather? Martha asked.It was getting late and she needed help getting the meal together. Ron Siepmann was famous for his Sunday morning pancakes.He’s in the field behind the shed, Richard said.The shed was across the road from the house, surrounded by a meadow of tall grass.Martha walked into the field, calling out for her dad. Hearing nothing, she turned around and headed back to the house. She opened the door to the shed, not expecting to find him.Ron Siepmann was lying face down on the floor. An ax lay nearby, and there was blood all around.Martha touched her father’s hand. It was cold.She ran to the road, frantic. Richard stood by the house with his aunt and three young cousins.”Richard,” Martha screamed. “Do you realize what you have done?”Richard’s face showed no emotion, but his hands started to twitch.”I stopped the spell after 127 years,” he said.Martha asked him what he meant.”Schizophrenia,” he said. “It runs in our family. Right, Mom?”It was another of Richard’s delusions.As Martha slumped to the ground, she saw splotches of blood on her son’s tennis shoes.***Alberta Lessard heard about what happened to Ron Siepmann on the news the next morning and it made her mad. “I suppose people are going to blame me,” she said later.Lessard said she never meant to make it harder for people who are sick to get care.She only wanted people who were misunderstood to have their side considered.There are lots of ways to get through to a person without “being a bully about it,” she said.When she was first teaching in a one-room school in northern Wisconsin in 1945, Lessard had a boy in her class named Sidney Anderson who would not talk. Everyone assumed he had some kind of disability.”I think today they would call that autism,” Lessard said.Sidney had been in first grade for three years, and his family was planning to send him to an institution.”I could hear him talking on the playground,” Lessard said.She worked and waited and finally, one day, after nearly a year, the boy spoke.”And, do you know what?” she said. “He could read like anything.”***On Sept. 9, a Friday, Lessard went to her bank in West Allis to withdraw her life’s savings. She said she had gotten a call the day before from a man from the Social Security Administration informing her that there had been a mistake and she owed the federal government $13,000.”I’m going to lose everything,” Lessard said later. “I won’t have any place to live. I won’t have any food to eat. Nothing.”She wanted to hide her money.But the bank manager would not allow Lessard to get the money without proper identification, and Lessard refused to leave.”I might as well die here,” she told him. “This is where all my possessions are.”The bank manager called the police.Normally, Mike Jungbluth, the West Allis police chief, would handle situations like this.Jungbluth, who started his career as a psychiatric nurse, first met Lessard 30 years ago when he was working at the mental health complex. He has a way of calming her down by bringing Twix candy bars to her apartment. He chuckles at her “ditties,” poems she writes in longhand chastising politicians, and he abides her fantasy of being the state’s attorney general.Lessard, who once ran from West Allis police, now relies on the chief to buy her food and help her cook.Jungbluth was out of town that day. Instead, two of his officers arrived at the bank. Eventually, they decided there was nothing else they could do.Two weeks after her 91st birthday, Lessard was arrested, put into a squad car and taken back to the Milwaukee County Mental Health Complex.It was her fifth arrest in two years and the 15th since 1996.Jungbluth figures Lessard has been arrested more than 50 times in the past 40 years at a cost of more than $400,000 in today’s dollars. When you factor in court costs and police time, the figure doubles.Lessard was assigned to a room on Ward 43-B – the same ward where two women had been sexually assaulted in 2009 by a patient with a history of violence who was allowed to roam the ward unsupervised.The following Tuesday, Lessard arrived in court for a hearing to determine whether there was probable cause to hold her at the hospital against her will. She looked tiny, slumped in a wheelchair wearing sweatpants, electric blue socks and a black windbreaker.The case was dismissed when the lawyer for the county withdrew his petition.She did not meet the standard that her famous case had established 40 years earlier.Before she left the courtroom, Lessard insisted on speaking. Patrice Baker, the court commissioner, obliged.For the next 52 minutes, Lessard delivered a monologue on everything from dirty deals between the publishing industry and public educators to the tragedy of veterans dying in the streets to her suspicion that the attack on the World Trade Center was “an inside job.”She explained how she was legally the attorney general of the state of Wisconsin and all public officials – including President Barack Obama and Gov. Scott Walker – were falsely elected.”I’m the top cop in the state,” Lessard said.***Martha and Jeff Wilson arrived at the Waukesha County Courthouse early on the morning of June 2 and sat in front. A few minutes later, the rest of the family arrived, taking up the next three rows. They smiled nervously at one another, smoothed their hair and checked their watches.At his initial appearance, Richard wore a padded olive-green sheath used when prisoners are considered such a high risk for suicide they might try to hang themselves with their own clothing. This time, he wore a standard-issue red T-shirt and pants.If Richard noticed his parents as he came through the door, he gave no indication. There was no nod or smile or shrug, no wince or frown or slumped shoulders – only a blank face.The prosecution read a brief report from the state’s psychiatrist concluding that Richard was too mentally ill to understand what was going on.He could not help in his own defense and, therefore, did not meet the criteria for standing trial.Waukesha County Circuit Judge William Domina declared Richard to be incompetent and committed him for treatment.Richard would be sent to Mendota Mental Health Institute, a maximum security detention facility for people who are criminally insane.Before he could be tried for killing his grandfather, Richard would have to be restored to sanity. The state’s psychiatrists would need all the help they could get in order to make that happen.So, on that day, Domina did something that the Wilsons desperately had tried to do for months.He ordered Richard to take his medicine.
© 2011, Journal Sentinel Inc. All rights reserved.
The story didn’t have any paragraphs when I pasted it on your webpage, so here is the link that will make it easier to read.
http://www.jsonline.com/news/law-creates-barriers-to-getting-care-for-mentally-ill-135387808.html
“It wasn’t hard for police to put Lessard back inside. All that was
required to commit a person to a mental hospital was an affidavit signed
by three people saying the patient was sick and in need of treatment.”
This is an awful way for things to be done and a law such as this is actually incredibly discriminatory as it was only applied to the mentally ill (and not the hypothetical diabetic I mentioned). We should not aspire to return to that. Not only does it open the gateways for an incredible amount of abuse, it ignores constitutional rights.
Once again: This not a strictly medical issue. If it were, dangerousness would not be the criteria; “could benefit from treatment” (what those horrid AOT laws use) would be. The push to turn it into a medical issue is one that should be fought and abhorred, not supported. Yes, it does involve someone’s health; but, more than that, it involves taking away a legal right and, because of that, it must remain a primarily legal issue. As it is a legal issue, furthermore, you must approach it as such: make a legal argument, not a medical one.
As I continue using the diabetic as an example, I would just like to further develop the situation for those who support changing the criteria:
A was diagnosed with Type 1 Diabetes at a young age. For most of his life, his parents have made sure he take his medication and participate in treatment. Though it kept the Diabetes at bay, it also came with unpleasant side effects that A did not appreciate. He wanted to treat it with ‘alternative medicine”, which he viewed as having less side effects. In addition, after awhile of not suffering from symptoms, he figured he must not have it that bad, anyways — maybe the doctors even made a mistake! As a consequence of all of this, on his 18th Birthday, A stopped taking his medication and sought out an alternative practitioner. His parents were horrified.
It did not take long for A’s condition to worsen. His blood sugar spiked, leaving him exhausted, his vision blurry, his feet tingling, unable to go long without needing to use the bathroom, he lost a significant amount of weight and he was constantly irritable and on edge. As he was feeling so sick, he missed quite a few days of class (he was in college pursuing his degree in another state; living in dorms) and his grades plummeted. Around this time, he also fell into a Diabetic Coma and, after being found half-dead by a stranger, was hospitalized. Upon discharge, he started taking his medication again; but, after a return of side effects, he quickly went off them. The cycle seemed bound to repeat itself.
His parents wanted to force him to take his medication and, if he started getting worse again, force him into the hospital before the coma occurred; however, as he was over the age of 18, there was nothing they could do. Should they be allowed to force him?
If you support AOT or a more flexible commitment for mental illness, then, by the reasoning many AOT-supporters put out, you should also support their right to force him to take medication — either inpatient or outpatient. If you do not support forcing this man into treatment but support forced treatment for mental illness, why? Why do you support less rights for the mentally ill or, depending on your viewpoint, why would you only want to take away the “barriers of treatment” for the mentally ill? If you do support forced treatment for A, why are you not advocating for it? Why don’t you fight for an AOT that is applicable to all illnesses?
(and noncomplaince is an issue in diabetes: http : // jama.ama-assn . org / content / 284 / 13 / 1709 . full – remove spaces or Google The Problem With Compliance in Diabetes, Medical Student JAMA)
One more thing…
As I speak of legal arguments, I would like to quote the 14th Amendment:
“1. All persons born or naturalized in the United States, and subject to the
jurisdiction thereof, are citizens of the
United States and of the State wherein they reside. No State shall make or
enforce any law which shall abridge the privileges or immunities of citizens of
the United States; nor shall any State deprive any person of life, liberty, or
property, without due process of law; nor deny
to any person within its jurisdiction the
equal protection of the laws.”
Note the equal protection part. Any forced treatment law that only applies to the mentally ill — including AOT — can be argued to be in breach of this as those with physical illnesses have a higher level of protection under the law.