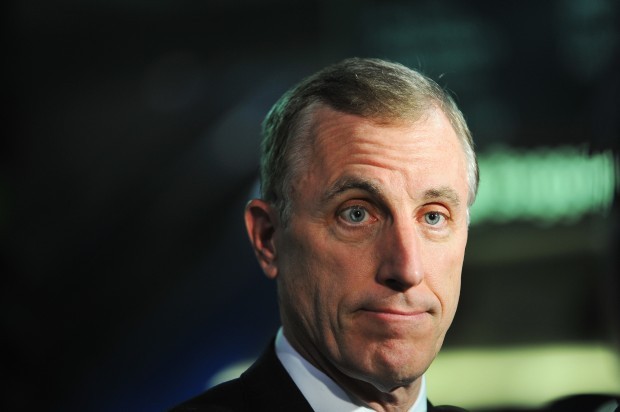
(3-17-17) My Monday blog, which questioned why Rep. Tim Murphy voted along party lines in support of replacing Obamacare with the Republicans health bill, didn’t sit well with the Pennsylvania Republican. Every major mental health group is opposed to the Republican plan because it will end Obamacare’s Medicaid expansion, which covers 1.2 million Americans with serious mental illness and substance abuse problems, as well as, scrap baseline coverage requirements. I am printing Rep. Murphy’s response to the criticism that he has received. It was first posted in The Hill newspaper on Thursday and also sent to me. Early today, the Hill published a response to Rep. Murphy’s. Tim Murphy – Republican Health Bill Fails People With Mental Illness was written by Dr. Richard G. Frank, PhD, the Margaret T. Morris Professor of Health Economics in the Department of Health Care Policy at Harvard Medical School. Here are the pro and con.)
Transforming Mental Health & Addiction Treatment: We’ve Only Just Begun
By Rep. Tim Murphy
As Congress delivers on the promise of delivering relief from the collapsing Affordable Care Act (ACA), we must be forward thinking and avoid re-purposing yesterday’s failed policies to solve today’s problems. In particular, we must include better strategies to advance mental health and addiction treatment.
While promising mental health and addiction insurance coverage, the ACA did little to provide real medical models of treatment for those suffering with mental illness and addiction. The evidence is staggering: skyrocketing rates of suicide and drug overdose deaths are now at all-time highs. Sadly, only lip service was paid to behavioral health by the previous administration’s whose agenda furthered the familiar pattern of limiting access to treatment, casting millions to the shadows of our healthcare system and dragging their feet on the implementation of mental health laws.
In a calculated move to save money in the Medicare program, the Obama administration attempted to strip the protected drug class status for life-saving psychiatric medications.
Following outrage from advocates and an explosive exchange I had with former CMS Deputy Administrator Jonathan Blum at an Energy & Commerce hearing, the cruel effort was abandoned. But the point was clear: mental illness remains a disease considered less important than physical disease.
In like manner, mental health and addiction coverage parity took a backseat. After a long-fought battle in Congress, President Bush signed the Mental Health Parity and Addiction Equity Act into law in 2008.
However, not until 2013 would the Obama administration implement parity, leaving millions of Americans with behavioral health conditions still fighting the insurance industry years after the bill was signed into law.
While the Health and Human Services Administration was churning out ACA-related regulation after regulation, Americans in mental health and addiction crisis were treated as second-class citizens.
The narrative regarding parity and mental health and addiction coverage under the ACA is frustratingly false. The Congressional Research Service, the Library of Congress’s nonpartisan research arm, confirmed the ACA, “did not modify or expand the federal mental health parity requirements.”
And state expansion of Medicaid simply resulted in many governors switching out state dollars for federal dollars. The National Alliance on Mental Illness noted in a 2015 report: “Both Ohio and Michigan, who expanded Medicaid by executive order, largely folded mental health services into Medicaid funding.”
With cuts to state mental health budget, however, advocates in both states are concerned that neither Medicaid nor the mental health system will meet the needs of individuals who remain uninsured and hard to reach.
House Republicans are offering a better way for health care with the American Health Care Act (AHCA), a law crafted with determination and thoughtfulness to further mental health and addiction treatment.
During the markup of the bill last week, questions were raised about the provision which sunsets the Essential Health Benefits for Medicaid Alternative Benefit Plans (ABP). While some criticize this as a cut to mental health and addiction treatment, a closer look reveals the truth. Under the AHCA, states are free to cover mental health and addiction treatment in their plans. If they do, existing parity laws – which I helped write – require mental health benefits to be provided at the same level, or “at parity,” with medical and surgical coverage in that same plan.
Beyond that, states have $100 billion from the Patient and State Stability Fund to provide treatment for behavioral health and addiction. Either way, patients will be provided robust mental health benefits with greater flexibility and in a more effective way. Consider, states such as Pennsylvania and West Virginia, hit particularly hard by the opioid epidemic, might decide to cover addiction treatment differently than Wyoming and Alaska, states experiencing the highest rates of suicide in the country.
States know best, and a patient-centered system is the solution. This is not a partisan battle. Our nation wants, and deserves, a system that works. The AHCA preserves two critically important components from the ACA for those with mental health diagnoses: the coverage of pre-existing conditions, including behavioral health conditions, and allowing young adults to stay on their parent’s health insurance until age 26 (75% of all lifetime mental health conditions onset before the age of 24).
Last session of Congress, Republicans stepped up to reform our nation’s broken mental health system. In his first interview as Speaker of the House, Paul Ryan told 60 Minutes that mental health reform was at the top of Washington’s “to-do” list. Months later, we delivered on that promise with the passage of the Helping Families in Mental Health Crisis Act, signed into law last December as part of the 21st Century Cures Act. But more work remains.
With a critical shortage of psychologists, psychiatrists and behavioral health workers, our outdated laws prevent access to real treatment. As a result, each year 350,000 Americans die of their mental illness.
We can and will do better.
Republicans will step up again to address the issues that the Obama administration overlooked in their failed health care reform endeavor, putting forth a health care plan that goes further than the current law to help families in mental health crisis. As we do, I will continue to roll out legislative solutions to provide treatment before tragedy.
We’ve only just begun.
Tim Murphy — Republican health bill fails people with mental illness
Representative Tim Murphy (R-Penn.) is correct in writing that helping people with mental illness is not a “partisan battle.” But we know he is someone who cares about this issue enough to realize this debate must be rooted in facts. The recent article Murphy penned for The Hill offers views that are at odds with basic facts and reality.
We think it is important to hold up some of the claims “of failed policies” in Congressman Murphy’s letter against the facts so that a more productive discussion of behavioral health policy can result. Moreover, the “better way” he argues that is offered by the American Health Care Act would make matters worse, not better, for the populations he champions.
Parity legislation and regulation: At the end of January 2010 the Obama Administration issued Interim Final Regulations for the Mental Health Parity and Addictions Equity Act. Those regulations had the force of law and covered the vast majority of points that appeared in the final regulations of 2013.
Moreover, starting in 2010 the administration trained Department of Labor inspectors and state insurance commissioner staff on the regulations in order to support enforcement and technical assistance efforts. The parity regulations improved the coverage for 103 million people starting in 2010.
The Affordable Care Act extended insurance coverage for mental health and substance use disorder treatment by including mental health and substance use disorders services as Essential Health Benefits that must be offered in the individual, small group and Medicaid expansion markets.
The ACA also extended the reach of the parity legislation supported by Congressman Murphy to require parity in individual, small group and Medicaid expansion coverage. The result was to expand coverage and the quality of coverage to about another 70 million people. Thus the total numbers that saw their coverage for behavioral health care improve was over 170 million. This is not exactly relegating behavioral health in the back seat.
The result of the efforts to expand and improve coverage was that about 1.84 million low people used services paid for through the Medicaid expansion and the Health Insurance Marketplaces. That directed estimated $5.5 billion new dollars annually towards treatment of behavior health conditions.
This is roughly five times the size of new spending called for in the 21st Century Cure Act that represented an historical increase in spending on substance use disorders. The well-being and support for people with mental illnesses and substance use disorders will not be advanced by the American Health Care Act that would result in a loss of insurance coverage for 24 million Americans many of who suffer from these illnesses (an estimated 29p percent). Nor will taking away $5 billion in treatment resources from the nearly 2 million people in treatment today improve the mental health of the nation.
Finally, claiming that the opioids epidemic reflects a simple failure of behavioral health policy of the last administration ignores the data on the trends in drug overdoses. The graph shows that the growing overdose problem pre-dates President Obama’s election. The trend data shows that the epidemic dates back to the Clinton and Bush administrations and is not the work of recent policy.
The loss of coverage for substance use disorder treatment that the American Health Care Act would cause would take away tools for fighting the opioid epidemic at a time they are badly need. Turning this on-going and changing national tragedy into a reflection on the important gains made over the last 10 years is a disservice to the importance of the challenge we must face together; we know that Congressman Murphy can do better.
Dr. Richard G. Frank, PhD, is the Margaret T. Morris Professor of Health Economics in the Department of Health Care Policy at Harvard Medical School. From 2009 to 2011, he served as the deputy assistant secretary for planning and evaluation at DHHS directing the office of Disability, Aging and Long-Term Care Policy. Dr. Sherry A. Glied is the Dean of New York University’s Robert F. Wagner Graduate School of Public Service and former Assistant Secretary for Planning and Evaluation in the U.S. Department of Health & Human Services.



