How America’s criminal justice system became the country’s mental health system
“I was very delusional, erratic, confrontational, and paranoid,” Kevin said. “So when they came, they tased me.”
It was not Kevin’s first run-in with police — and it wouldn’t be his last. But it’s the one Kevin and his father share as one of his worst experiences.
But Kevin also knows what it’s like to have a much better type of encounter — one that doesn’t just resolve the current issue but also helps make sure something like it never happens again.
In Kevin’s last serious encounter with police in 2006, he was staying at a safe house, where people with mental health problems could relax for a night. There, he took off his clothes — thinking it made him invisible — and walked outside.
A police officer, with training for mental health crises, approached Kevin. Kevin was scared, remembering the last time police approached him (and tased him). But this officer talked softly, reasoned with him, and, finally, convinced him to get into the car — no violence necessary.
The cop didn’t take Kevin to jail — he took him to a hospital. There, Kevin got a case manager. She fended off criminal charges, got Kevin into a “housing first” program for aid, and helped him sign up into a jobs program where he learned to become a peer-to-peer support specialist.
With proper care and medication, Kevin has not had a dangerous run-in with police in the nearly 10 years since.
“He finally got the help he needed, in part because a crisis intervention team–trained officer and a case manager” treated him as a mental health patient, Pete said.
These two scenarios, law enforcement officials and advocates say, show what happens when police — and the justice system more broadly — are equipped to deal with people with mental illnesses: While the first encounter ended in a violent arrest that actually amplified Kevin’s paranoia toward police, the second was resolved peacefully in a way that prevented potential violence in the future.
Unfortunately, the non-peaceful resolution remains horrifyingly common in America. And while this issue often shows up in the justice system, it reflects a much broader failure in US policy and society.
Police often respond to mental health crises — and shoot the patient
/cdn0.vox-cdn.com/uploads/chorus_asset/file/3537446/459617770.0.jpg) Jewel Samad/AFP via Getty Images
Jewel Samad/AFP via Getty ImagesIt’s a terrifying statistic: Someone with an untreated mental illness is 16 times more likely to be killed by police than other civilians approached or stopped by law enforcement, according to a 2015 report by the Treatment Advocacy Center.
Kevin was lucky in that he was never actually shot by police. But he had several close encounters, as he and his father described to me.
One encounter began shortly after a psychotic episode that briefly landed him in an emergency room in 2002. Within 48 hours, Kevin wrapped tinfoil around his head, claiming that the CIA was reading his thoughts. He slipped out of the house and broke into a stranger’s home to take a bubble bath, and eventually several officers and a police dog helped arrest him and take him into custody.
Kevin received some care after that encounter, albeit under the threat of jail time. But he eventually relapsed, leading to the encounter in which police used a stun gun to arrest him, and the final incident in which a police officer with mental health crisis training helped get Kevin longer-lasting care.
But it’s troublingly easy to imagine a scenario in which Kevin’s story turned out differently.
Two parents, Gregory and Sigrid Lambert in New Hampshire, told me a very different story. Police shot and killed their son, Harrison, who had borderline personality and schizoaffective disorders, in 2015, following several encounters with law enforcement.
Gregory told me the story of the final encounter:
Harrison started having a mental breakdown, and he threatened me with a knife — two times. The second time, I was in the house, trying to blockade him from coming into my bedroom. I said that I’m going to wait until his mother comes home. [At the time, Harrison responded that he will “take care of her” when she does.] I said, well, I need to get help here.
So I made the call, per what the mental health counseling service told me to do, to call 911.
After roughly about two minutes, the police were here. I was still inside, talking to the 911 dispatcher. During that time, I heard about four shots. I ran out the door, and Harrison was laying on the ground.
Harrison died the following morning. The New Hampshire Union Leader reported that the shooting was deemed justified, since Harrison charged at the police while armed with a knife. The parents insist police could have used a stun gun or shot Harrison in the leg, but police argued that’s not standard protocol.
“It’s the most horrible thing a parent can go through,” Sigrid said, her voice cracking.
The lesson, the Lamberts told me, is that they shouldn’t have called the police for help. But when I asked them what else they could have done, their voices grew strained. They were clearly exasperated by the lack of good answers.
“It would have led to him breaking down the door and me defending myself. I wouldn’t have killed him, but I would have knocked him right out,” Gregory said. “I didn’t want to go physical.”
“Yeah,” Sigrid responded, “but what else could you do?”
Such encounters with police aren’t atypical for people with mental illnesses. As the National Alliance on Mental Illness (NAMI) found, each year 2 million people with serious mental illnesses are admitted to US jails.
The experiences of the Earleys and Lamberts reflect how this can happen — and how some encounters can go horribly wrong. Very often, a psychotic episode will result in someone calling the police. Depending on the circumstances of the situation — what is happening, whether someone is at risk, how the person is behaving, the cop’s mood, training, and interpretation of the events — it can lead to no arrest, a peaceful arrest, or use of force to arrest or stop someone.
That’s not an accident. Over the years, America has depleted the public mental health system. As a result, cops are often the first responders to mental health crises — even when they don’t have the training for it.
The system responds to mental health crises
only after it’s too late
If people were getting comprehensive care and support, police most likely would not need to get involved in many of the circumstances that end up in horrible tragedies. But very often in the US, that’s not happening.
Before Kevin broke into a neighbor’s house and was arrested by police, Pete tried to take steps that would have prevented the whole encounter. Kevin had just suffered a psychotic episode in 2002, and Pete raced Kevin to emergency care to hopefully get Kevin into some form of long-term care, potentially against Kevin’s will if necessary.
(Pete, a journalist, wrote about the full experience in his 2007 book, Crazy: A Father’s Search Through America’s Mental Health Madness, and continues to write about the issue on his blog.)
But doctors said they couldn’t do anything because Kevin, an adult, didn’t appear to pose a threat to himself or others in the four hours they sat in an emergency room. So he was let free, and within 48 hours, he went through the episode in which he broke into the neighbor’s house.
“Under state law at the time — this was before the Virginia Tech shooting — you had to be an imminent danger to yourself or others before you could be required to undergo any kind of treatment against your will,” Pete said. “And the fact we had been sitting there for four hours showed there was no danger.”
The problem with this kind of standard, according to advocates, is that people with mental health issues can be unpredictable. They can display some warning signs — as Kevin did with the psychotic episode that led to the emergency room visit — but whether they’ll become an actual danger is hard to say.
And since people with mental health issues may not be able to comprehend everything happening when they have an episode, they won’t necessarily check themselves in for their own safety — even if a real problem is imminent.
In Kevin’s case, when police arrested him the system’s first instinct was not to check him into treatment. Instead, police told Pete that Kevin would need to pose a direct threat to someone for that step to be taken. So Kevin was threatened with jail time. “The guy told me to do what my conscience told me to do,” Pete said.
Exasperated, Pete decided to lie, telling authorities Kevin threatened to kill him. Pete said this bought time until Kevin finally voluntarily checked himself into a hospital, upon his attorney’s advice.
Kevin took his medication while on two years of probation for breaking into the stranger’s house. But after the probation period ended, he stopped taking his pills and started acting out again.
Kevin said he abandoned his medication because he didn’t believe the drugs were helping him: “You feel like, ‘Okay, well, maybe I had an episode. But maybe I don’t really have this thing that’s going to be lifelong. Maybe it was just a freaky occurrence.’ … It’s very hard to come to terms with the fact you have a mental illness, so lots of people are in denial.”
The next episode came. Pete tried to call a mobile crisis response team, an emergency health unit in Fairfax, to try to prevent yet another encounter with police. Pete hoped they could evaluate Kevin and help him get back on his medication without getting the police involved.
Help didn’t arrive, Pete said:
I said, “My son is off his meds. He’s starting to slip. Please come over.”
They said, “Is he dangerous?”
I said, “No, not yet. But here’s what happened before…”
They said, “That’s not fair. You can’t judge him based on what happened in his past. Please call if he’s dangerous.”
He tried again at night, once Kevin became violent:
Well, at night he became violent — the night I didn’t have to lie. I called the same dispatcher and said, “My son’s violent. Please come.”
They said, “Wait a minute. Is he dangerous, or is he violent?”
I said, “He’s violent.”
They said, “We don’t come if he’s violent. Call the police.”
Once again, the response came only after a crisis, and police had to get involved.
This is a theme you hear again and again when talking to people with mental illnesses, their parents, and advocates: The system often refuses to respond until it’s too late. It took a chain of events that began with Kevin breaking and entering to hospitalize him. It took an actual threat of violence to get someone to respond — and even then only police could show up, once again putting Kevin at risk of deadly police force and jail or prison time.
The criminal justice system has picked up
the slack for the mental health system
At the root of all these encounters is a bigger problem: Mental health care is woefully underfunded in America, and the criminal justice system is often the only institution that can pick up the slack.
As a result, about 15 percent of men and 30 percent of women booked into jail have a serious mental health condition, most of whom don’t get needed care while they’re in jail, according to NAMI.
There are myriad reasons the system works this way. To some extent, there are concerns about civil liberties: Should someone really be forced into mental health care just because family members think he’s dangerous or violent? And what, exactly, qualifies as violent or dangerous in these scenarios?
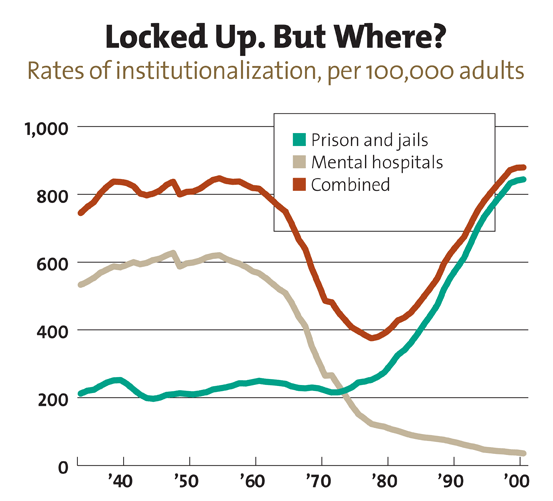
These fears are particularly pronounced by the abuses exposed in the mental health system throughout the 1960s and 1970s, which have been ingrained in the American psyche by popular media like One Flew Over the Cuckoo’s Nest.
But mental health treatments have improved since then. Yet police and the criminal justice system are still, more often than not, the first responders to mental health crises.
This is the result of decades of policy: As different levels of government slashed resources to mental health care, the justice system was left as the only institution equipped to respond.
It’s getting worse. In multiple report cards, NAMI outlined some of the cuts that followed the Great Recession: None of the states graded by NAMI earned an A, and almost all made significant spending cuts to mental health services in the past few years. And these cuts came to a system that NAMI had already criticized for decades as being severely underfunded.
The result, as outlined by a 2014 national survey by the Treatment Advocacy Center: “Not only are the numbers of mentally ill in prisons and jails continuing to climb, the severity of inmates’ illnesses is on the rise as well.” Ultimately, the survey found that the number of people with mental illnesses in prisons and jails outnumber those in state hospitals 10 to 1.
These prisons are supposed to provide some semblance of care to inmates. But as the Treatment Advocacy Center found and other advocates can attest to, that’s simply not the case. Often, jails and prisons just don’t have the resources to do so. According to NAMI, at least 83 percent of jail inmates with a mental illness do not have access to crucial treatment.
It’s worth noting that most people with mental illnesses are not violent. Many are locked up for low-level crimes — loitering, littering, criminal trespassing, and drug possession. Indeed, people with mental illness are more likely to be victims — not perpetrators — of violence. And only about 3 to 5 percent of violent acts in the US are carried out by people with serious mental illnesses, while about 4.2 percent of adults in the US experience a serious mental illness in a given year that substantially interferes with or limits a person’s major life activities.
Still, some people with serious mental health issues can have dangerous crises. And the gaps in funding have turned police officers into the first responders to such episodes.
“Oftentimes, people who are psychotic are willing to try to get help, but our system is set up not to really help them, not to make it easy until you get arrested,” Pete said. “And then you’re stuck in the criminal justice system, which inflames the situation.”
What’s more, this comes at a tremendous cost to the justice system. In his testimony to Congress, Florida Judge Steve Leifman laid out the costs he saw firsthand:
Several years ago, the Florida Mental Health Institute at the University of South Florida completed an analysis examining arrest, incarceration, acute care, and inpatient service utilization rates among a group of 97 individuals in Miami-Dade County identified to be frequent recidivists to the criminal justice an acute care systems. Nearly every individual was diagnosed with schizophrenia, and the vast majority of individuals were homeless at the time of arrest.
Over a five year period, these individuals accounted for nearly 2,200 arrests, 27,000 days in jail, and 13,000 days in crisis units, state hospitals, and emergency rooms. The cost to the community was conservatively estimated at $13 million with no demonstrable return on investment in terms of reducing recidivism or promoting recovery. Comprising just 5 percent of all individuals served by problem-solving courts targeting people with mental illnesses, these individuals accounted for nearly one quarter of all referrals and utilized the vast majority of available resources.
It should be no surprise, then, that spending more on mental health care can actually save money, on top of proving more effective at treating a patient.
A 2013 review of the research by the Vera Institute of Justice, a nonprofit organization that works on public safety and justice issues, found that “it can cost two to three times more for a person with serious mental illness to become involved in the criminal justice system compared to receiving treatment in the community.” And, the review found, some mental health programs led to fewer arrests and shorter jail stays among mentally ill populations.
It isn’t ideal to keep any of these issues in the criminal justice system’s jurisdiction. Advocates, like the Treatment Advocacy Center, would like to see a stronger public mental health system — one that prevents a mental illness from getting so bad that it requires a criminal justice intervention. But until that happens, the best option might be to build the criminal justice system to more sensibly deal with mentally ill people.
Training police to do better
While no one seems to like this setup, the reality of its existence has driven some law enforcement officials to change their ways at the urging of advocates. This is, to some extent, a bit of harm reduction: No, police should not be the ones responding to mental health crises. But given the reality of the situation, police should be trained to deal with these crises properly.
I spoke to several people across the country who train police officers in mental health training, which is also known as crisis intervention training: Dixie Gamble of Tennessee,Paton Blough of South Carolina, and Sherry Cusumano of Texas — all of whom have worked with NAMI and police. All of them emphasized empathy and deescalation.
Police, for example, may not understand that people going through psychotic episodes genuinely aren’t in control of their actions at the time. “You think you’re in control when you’re really not,” Blough, who has bipolar disorder and has experienced several bad run-ins with police, said. “That’s the delusion of the illness.”
But if police know someone isn’t in control of their actions, it makes deescalation seem much more sensible. After all, why would you shoot someone — effectively punishing them — for something they can’t help?
Through deescalation, officers try to level with people in the middle of a mental health crisis. In doing this, officers should keep their distance and calmly talk to the person they’re approaching to try to get them to relax. The idea is to get the person to trust the officer, eventually convincing the person to submit without any violence.
“Deescalation is always the intention,” Gamble said. “When the officer shows up, ask basic questions in a soft, lower voice.” She added, “Instead of putting your hands on the gun, hold your hands down by your side, open your palms outward, and ask simple questions: ‘Dude, are you okay?’ or, ‘Ma’am, are you okay?’ Simple, right? ‘What is your name?’ ‘What would you like?'”
From that point, officers should proceed to subdue the person by calmly talking them down and eventually linking them to health care.
This can even involve the officer acknowledging, but perhaps not accepting, a person’s delusions. For instance, if someone in a psychotic state thinks he’s the president, don’t argue about whether it’s true. “Go along with it,” Gamble said. “The idea is that as long as that person is talking and not doing, you’re deescalating.”
This can be safer not just for the person in a mental health crisis, but for the cop, too — since it makes a person in the middle of a crisis less likely to lash out.
But very often police are trained to essentially do the opposite of what they should.
“Police departments are trained to be authoritative — to step in, then take charge,” Pete Earley said. “You’re dealing with someone who’s psychotic, who’s already paranoid, who may be hearing voices that people are trying to hurt him. When someone encounters a police officer like that, it’s a recipe for disaster.”
This gets to the heart of the problem with how police respond to such encounters: It’s not that cops go into these situations with bad intentions, but rather that they’re essentially trained to handle these situations poorly. By changing that training, then, cops can go into crises with a better idea of what to do — and possibly avoid a deadly encounter.
Coupled with this training, some local and state governments have adopted diversion programs that try to route people with mental illnesses to care instead of to prison and jail. Many places have embraced mental health courts that link someone who’s likely prison-bound to community-based mental health care. Fairfax County, Virginia, where the Earleys live, adopted a jail diversion program that moves low-risk offenders with mental illnesses to community-based care, which could have prevented many of the bad run-ins Kevin had with police by getting him care earlier.
One major problem: Although these policies can save money in the long term, they can require a big initial investment and culture shift. For lawmakers and law enforcement officials, the cost remains the largest hurdle: a big commitment to a policy they’re not all convinced is necessary or will work.
Nonetheless, these policies are gaining momentum across the country — to good effect.
How one county is trying to do better
Some law enforcement officials have pushed ahead with reform. In Cook County, Illinois, the sheriff’s department has taken steps to both reshape police training and the local jail — the sheriff oversees the county jail — to make up for a lack of resources in the area, which includes the city of Chicago.
The current sheriff, Tom Dart, did not come at this easily after taking office in 2006. In 2008, the US Department of Justice found startling, unconstitutional conditions at the county jail — leading to a reform agreement that the sheriff’s office says it’s now in full compliance with. In 2012, Chicago Mayor Rahm Emanuel led the charge to close six of 12 city-run mental health clinics, stranding thousands of patients without care.
At the same time, as many as one-fourth of the jail’s roughly 8,200 inmates have mental illnesses.
These circumstances led Dart to make stronger mental health policies his big cause. As one example, Dart, who often calls his jail the largest mental health facility in the country, wrote a scathing op-ed for the Chicago Tribune calling on the nation to “stop the criminalization of mental illness.”
Dart has made several changes to this effect: He appointed a psychologist to run the jail. He started a program that connects people with mental health services, teaches them how to cope with their mental illnesses, and follows up with ex-inmates after they’re released from jail. His office even plans to run a mental health clinic in Chicago — to make up for the city shutting down half of its clinics.
“If I’m going to have society be so indifferent to the mentally ill that it dumps them in jails for virtually no reason, I’m not going to sit by and just treat them in a traditional way that you would people who enter jails,” Dart, who was previously a prosecutor and state legislator, told me. “I’m going to treat them as if they’re entering a hospital instead. I treat them all with dignity, but treat them as a person with an illness, which they do have.”
For Dart, this is quite simply the right thing to do. “It was morally wrong to do what we were doing,” Dart said. “Society as a whole, we should be embarrassed about what we are doing.”
But he added, “Say for some strange reason you want to toss the moral issue out the window. Talk about the fiscal side of it. How does it make any sense fiscally to be locking up someone who’s ill — who committed a crime in the loosest sense of the word — to lock them up in a setting [where] they cannot conceivably make their illness better, and their illness ensures their coming back in here? That’s an outrageously expensive proposition.”
Since many of Dart’s programs are early, it’s hard to evaluate their full effects — but studies of other programs, as the Vera Institute’s report noted, suggest it is saving money over time. And many inmates seem to like the program, based on interviews withVice News and the Atlantic.
Other facilities seem to be paying attention, too: Dart said officials from other jails, including New York City’s Rikers Island and Los Angeles County, have reached out to him to see how they can follow his model — to the point that his office has drafted a letter to help guide other jails and prisons around the country.
Dart has applied this reform-minded approach to his sheriff’s deputies, too. According to Dart’s office, about 70 percent of the sheriff’s police officers have at least 40 hours ofcrisis intervention training. In comparison, only about 15 percent of Chicago officers have similar training, according to the Associated Press.
Dart quickly admits not everything is perfect. There are still serious questions about some of the conditions and sanitation in the county jail. And Dart said he wants to continue expanding the programs he’s built. “We’re not done by any stretch,” he said.
But as the country as a whole continues neglecting mental health care more broadly, Cook County’s model might be a sign of the future.