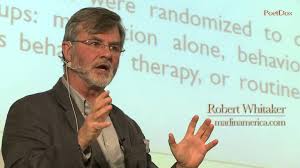
In the past two decades, Robert Whitaker has published books and articles that challenge the conventional wisdom about the widespread use of medications in treating mental illnesses. A research paper entitled: The case against antipsychotic drugs: a 50-year record of doing more harm than good, that the journalist/author published in 2004 is representative of the skeptical eye that Whitaker casts.
By chance, I was included in an email exchange where Whitaker objected to being labeled as someone who is unilaterally “against” medications. Dr. Allen J. Frances, Professor Emeritus of Psychiatry and Behavioral Sciences at Duke University Medical School, suggested that Whitaker clarify his views. In this guest blog, Whitaker explains what his research has shown him.
Me, Allen Frances, and Climbing Out of a Pigeonhole
All of this led to my having an email exchange with Allen Frances, who urged me, if I indeed thought antipsychotics had a use, to make this publicly known. My writings on this topic, he wrote, had:
“Caused collateral damage in 2 ways: 1) misleadingly discouraging meds for those who have tragic outcomes without it, and 2) contributing to the adversarial relationship between service users vs providers & families that is unique to the US and a major reason our system is such a mess. I am absolutely frank with you because I think you are intellectually honest and well meaning, but also unbalanced by the pressures of leading a crusade and by a lack of clinical and life experience with the constituency whose needs you ignore. With relatively small changes in the emphasis of your message and a clarification that you support selectivity, you could broaden your mandate to include the needs of the severely ill inappropriately in jail & homeless and could help heal the rupture between users and providers & families. I understand that you haven’t caused the problems and the limitations of any one person in healing them, but you are in a unique position to help and I think it would be irresponsible of you not to try once you fully understand the other side of the story you are presenting.” (Quoted with Allen Frances’ permission.)
Pete Earley also wrote to say that if I wrote such a piece, he would like to publish it on his site.
Now, my first response was to point out the obvious, as I did in my reply to Dr. Frances: I think his understanding of my “influence” is greatly exaggerated. My second response was to shake my head in wonder: That is quite the paragraph! But then I began grappling with whether to respond to his request to declare that I “support selectivity” in the use of antipsychotics.
It was, after all, a request that, at the outset, puts me into a pigeonhole not of my own making (anti-med), casts me more generally in an unflattering light (my work is misleading, unbalanced, irresponsible, and so forth), and then asks me to do something I never do, which is express my opinion, to “service users,” on how antipsychotics should be used. I have an opinion on what the scientific literature has to say about the use of antipsychotics, but that is a very different thing. The latter reflects the source of my writings on this subject, and its limitations.
Plus, I have written about my thoughts on this many times: I think the scientific literature argues for using antipsychotic medications in a selective manner that seeks to minimize their long-term use.
However, while I was dithering on whether to publicly respond, Allen Frances wrote a blog on the Huffington Post titled “Psychiatric Medications are Not All Good or All Bad.” There were pro-medication fanatics, and anti-medication fanatics, and Allen Frances, in his private email to me, was in essence asking me to climb out of the anti-medication fanatic camp (my pigeonhole), and join him and Virgil Stucker, from the Foundation for Excellence in Mental Health, in this “middle way” camp.
Having read this, I can now see a reason for responding, as it can help put the issue that society needs to address into clear focus. In his “middle way” piece, Allen writes that psychiatric medications are “very helpful” when prescribed for “clear-cut psychiatric disorders.” In his view, the problem with our societal use of psychiatric drugs is that they are overused, and that it is when they are prescribed to people without any real disorder that they cause harm. This is a critique that is entirely consonant with the conventional narrative: the drugs are effective, and the problems arise from poor prescribing practices. There is nothing in that critique that challenges conventional wisdom.
I think the issue is of a very different sort. I think science is telling us that antipsychotics, on the whole, worsen long-term outcomes, even when prescribed for “clear cut psychiatric disorders,” and thus, if psychiatry wants to develop evidence-based protocols, it needs to figure out how to minimize their long-term use. And that is a belief that directly challenges the conventional wisdom, and calls for a very different response.
Although this is going to make for a long blog, in order to respond to Allen Frances’ request, I think is important to once again detail my “journey” through scientific literature. It takes time to reject a conventional narrative and see the world in a new light.
Step One: Mad in America
As I have often written before, when I first dove into this subject of psychiatry, while co-writing a series with Dolores Kong for the Boston Globe, back in 1998, I did so with a conventional understanding of antipsychotics. Our reporting took place within a societal narrative that went like this: Antipsychotics were an essential treatment for schizophrenia and other psychotic disorders. They fixed a chemical imbalance in the brain, and thus were like “insulin for diabetes.” These drugs kicked off a psychopharmacological revolution, a great advance in care. Their discovery in the 1950s made it possible to close the mental hospitals, as the severely mentally ill could now live in the community. And, if patients didn’t want to take the drugs, that was because they lacked insight into their disease, and didn’t know the drugs were good for them.
Given that context, Dolores Kong and I wrote, in one part of the series, about how unethical it had been for psychiatric researchers to have conducted studies in which antipsychotics were withdrawn from schizophrenia patients. Would a study ever be conducted where insulin was withdrawn from a diabetic?
The one nettlesome factor for me, when we wrote that series, was that when I called up David Oaks of Mindfreedom for a quote, expecting him to say how awful such studies were, in that they took away helpful treatment, he said instead that there was good reason for “patients” to hate those drugs, and stop taking them. They often made people feel like zombies, he said, and then he added something about the drugs causing “brain damage.” I then called up a “thought leader” to ask about this, but he assured me that while antipsychotics did have side effects, the people who didn’t like them didn’t understand that they were sick and thus needed the medication, and as for the drugs causing brain damage, if anything it was untreated psychosis that caused brain damage, and the drugs helped protect against that.
But Oaks’ words stuck with me, a seed of doubt had been planted, and after I got a contract to write Mad in America, I came to see that there was a “counter-narrative” that could be investigated. If there was anything evident in a study of the history of the treatment of the “seriously mentally ill,” it was that the “mad” patients regularly saw the treatments forced on them in a different light than those who prescribed the treatment. There were competing narratives, and that remained true in the modern pharmacology era. In the conventional narrative told to the public, antipsychotics are characterized as a great medical advance. Then there is the counter-narrative told by many who had taken the drugs (and often forced to do so). And here is what I found while writing Mad in America: when you hold up these contrasting narratives side by side, history and science provide reason to conclude that the patient narrative has much merit, and give the lie to the conventional one.
Every important detail from the conventional narrative, which tells of a great medical advance, can basically be filed under the heading of “not really true.” The arrival of the antipsychotics into asylum medicine did not lead to deinstitutionalization; a change in social policy did. The dopamine theory of schizophrenia arose from an understanding of how drugs acted on the brain, and not from an understanding of what was going on in the brains of people so diagnosed, and when researchers looked to see whether people diagnosed with schizophrenia had overactive dopamine systems as a matter of course, they didn’t find that to be so. The drugs were not like insulin for diabetes. Nor was there evidence that the arrival of the antipsychotics kicked off a great advance in outcomes for schizophrenia patients. Indeed, in a 1994 paper, Harvard researchers reported that long-term outcomes were now no better than they had been in the first third of the 20th century, when water therapies were a mainstay treatment.
In contrast, a scientific understanding of antipsychotics supported the patients’ counter-narrative. Thorazine, Haldol, and other first-generation antipsychotics powerfully blocked dopamine pathways in the brain, which reduced one’s capacity to respond emotionally to the world and to move about it. Hence the zombie feeling. Antipsychotics did cause brain damage, as could be seen in the twitchings of people who developed tardive dyskinesia after years on these drugs. Moreover, research had shown that in compensatory response to the drug’s blockade of dopamine receptors, the brain increased the density of its dopamine receptors, and, there was reason to worry that this increased the person’s biological vulnerability to psychosis. Given these facts, there was plenty of reason for people diagnosed with schizophrenia and other psychotic disorders to want to stop taking them.
In terms of the “evidence base” cited by psychiatry for its use of the drugs, which is held up by psychiatry as its trump card in this battle of narratives, it is easy to see that the evidence for long-term use is flawed. Researchers had conducted any number of studies in which a group of stabilized patients were either maintained on an antipsychotic or abruptly withdrawn from the drug, and with great regularity, the drug-withdrawal group relapsed at a higher rate. This was seen as proving that continual drug use lowered the risk of relapse, and thus provided evidence for maintaining patients indefinitely on the medication. But, of course, another conclusion to be drawn is that the high relapse rate is a drug-withdrawal effect, and not evidence of the long-term risk of relapse in unmedicated patients. The relapse studies also didn’t provide any evidence about how well schizophrenia patients functioned on the drugs, or their quality of life, particularly over the long term.
As such, while writing Mad in America, I came to think that the problem with antipsychotics was that their use arose from a false narrative, as opposed to good science. Conventional antipsychotics needed to be seen for what they were: as agents that blocked dopamine receptors, which produced a cascade of effects. One effect, it could be argued, was that this blockade reduced psychotic symptoms better than placebo over the short term. Other effects of antipsychotics were decidedly negative, and as for long-term use, the evidence cited for this was flawed. Any helpful prescribing of the drugs would need to be done with that clear-eyed view of the science, and, most important, with a willingness to listen to the thoughts of those who were prescribed them. But the field had painted a picture for society of medications that were curative and essential, and in order to maintain that story, the field had to dismiss the protests of patients as evidence of anosognosia.
That was the history told in Mad in America. The book wasn’t about whether antipsychotics were “good” or “bad,” but about the story told by psychiatry about the drugs (to society and to itself). It was that false storytelling, together with the dismissal of the patients’ subjective experiences on the drugs, that was a prescription for using the drugs in a way that did harm. The false storytelling—as the subtitle of Mad in America suggested—led to “bad medicine.”
As for the merits of the newer atypical antipsychotics, when Mad in America was published (2002), the new “atypicals” were being presented as a great advance on the first-generation antipsychotics. At that time, I believed that it was too early to know whether that was so, particularly since this “advance” could not be found in the trial data submitted by the makers of the atypicals to the FDA, but only in the articles published by researchers paid by the pharmaceutical companies to conduct the clinical trials. So, it seemed to me, the jury was still out on whether the atypicals would prove to be so great, and as subsequent government-funded studies revealed, the data submitted to the FDA proved prophetic. The new drugs could not be said to be an advance on the old.
Step Two: Anatomy of an Epidemic
In Anatomy of an Epidemic, I focused specifically on this question: What did the research literature reveal about the long-term effects of antipsychotics and other classes of psychiatric medications? Did they improve the long-term course of schizophrenia, depression, bipolar disorder, and other such major disorders? Or not? What did psychiatry’s own research show?
Moreover, I wasn’t intent on investigating whether the benefits of a class of psychiatric medications outweighed their risks. I wanted to see what the literature revealed about their long-term effects on the benefit side of the equation only. Did the literature show that the medications reduced the target symptom of the disorder over the long-term? Did they improve functional outcomes? For a class of drugs to be seen as “effective,” there has to be something on the benefit side of the risk-benefit analysis, as otherwise there are only aggregate risks to be tallied up. And I wanted to see if such benefits were visible in the scientific literature.
Now, when you focus on that question, you have to dig out a history of science, which stretches back to the years before the introduction of Thorazine, but suffice to say, by the end of the 1970s, leaders of the NIMH had expressed a concern that antipsychotics might have the perverse effect, over the long-term, of making patients more biologically vulnerable to psychosis than they would be in the normal course of the illness. This worry arose from aretrospective study conducted by Samuel Bockoven, and by three long-term studies funded by the NIMH, and was expressed by William Carpenter, one of the leading authorities in schizophrenia research. In addition, there was growing concern about the frequency with which medicated patients were developing tardive dyskinesia, and this led Jonathan Cole, who was then head of the NIMH’s Psychopharmacology Service Center, to write an article provocatively titled: “Maintenance Antipsychotic Therapy: Is the Cure Worse than the Disease?”
This worry arose at the same time that researchers were discovering how the brain, in order to compensate for the drug’s blockade of its dopamine receptors, increased the density of these receptors. Two Canadian researchers then argued that this drug-induced dopamine supersensitivity could lead to more severe psychotic symptoms, and severe relapses upon drug withdrawal. Thus, after 25 years of studying antipsychotics, researchers had come to a stunning possibility: These drugs might worsen the very symptom they were designed to treat, and that was apart from all of their other adverse effects.
As a discipline, psychiatry soon put that concern out of mind, or at least pushed it away from the forefront of its concerns. Then the atypicals arrived in the 1990s, and soon the field was convincing itself that the new drugs were markedly better than the first generation drugs, and would produce profoundly better long-term outcomes.
But although psychiatry may have pushed worry about drug-induced dopamine supersensitivity out of mind, in Anatomy of an Epidemic I kept that concern—and other related concerns about their long-term effects on functional outcomes—front and center. Thirty years had passed since that worry was first raised, and thus there was plenty of new research that could be reviewed, and what I found was this: A review of such studies, time and again, provided reason to think that antipsychotics were worsening outcomes in the long-term (in the aggregate). MRI studies by Gur and Andreasen showed that the drugs caused changes in brain volumes that were associated with a worsening of positive symptoms, negative symptoms, and functional impairment. The World Health Organization, in two cross-cultural studies, reported that schizophrenia patients in three developing countries had markedly better outcomes than in the U.S. and other developed countries, and that in those poor countries, only a small percentage of patients—16%—were regularly maintained on the drugs. Philip Seeman’s animal research led him to publish a paper on why antipsychotics fail over time, and it was because the drugs induced an increase in dopamine receptors with a “high affinity” for the neurotransmitter. Then came Martin Harrow’s long-term study, in which the patients who stopped taking medications had markedly better outcomes starting at 4.5 years. This evidence was of many different types—MRI studies, cross-cultural studies, animal studies, and a long-term naturalistic study—and it was all of a piece. And thus a coherent scientific narrative, stretching across fifty-five years, emerged: a worry about the long-term effects of antipsychotics arose within the first twenty-five years of their use, and evidence of many types since then confirmed that initial worry.
Now, given that evidence, what does that say about the “best use” of these drugs? That is a question that psychiatry, the mental health establishment, and society should discuss. But it is a discussion, I believe, that should begin with a full airing of the scientific literature.
If one wants to think “categorically” about this evidence (and in fact, “evidence-based medicine” regularly encourages categorical thinking), then an argument can be made that, if the drugs indeed worsen outcomes in the aggregate, then they shouldn’t be used long-term. The evidence calls for the development of some other form of treatment and care.
But that is an argument to be made by others. My own thinking, as I sought to write about solutions in the final part of Anatomy of an Epidemic, was this: at the very least, the “evidence” argued for a selective-use model, one that would involve trying to help first-episode patients recover without the use of antipsychotics, and for those prescribed the medications, there still needed to be an effort to minimize their long-term use. That was a model that could still take advantage of the drugs’ “short-term” efficacy in certain patients, and also provide for long-term use in patients that didn’t seem to do well without the medications. And so I scoured the research literature to see if there were any reports of a provider using antipsychotics in that manner, and that brought me to the research papers published by the Open Dialogue group in Tornio, Finland. They used antipsychotics in precisely that way and they told of five-year outcomes that were dramatically better than the norm in the United States and other developed countries, where the standard is to maintain schizophrenia patients on the drugs as a matter of course. For me, that program served as a “proof of principle”: the research literature showed that the use of antipsychotics needed to be rethought, and the Open Dialogue results told of the vastly improved outcomes that could be achieved by doing so.
Step Three: Post Anatomy
The first edition of Anatomy was published in 2010, and since then new research has been published relevant to this question. The evidence showing that antipsychotics shrink the brain has grown more robust. Philip Seeman published another paper on how both an atypical antipsychotic and a first-generation antipsychotic induced the dopamine supersensitivity that, in his animal models, led to the failure of antipsychotics over time. Martin Harrow published his 20-year outcomes, and published more detailed analyses of the better outcomes for the unmedicated patients. In one article, he reported that medication-compliant patients were much more likely to be psychotic over the long-term than those who got off the drugs early on and stayed off them, and he discussed whether drug-induced dopamine supersensitivity was a reason for that remarkable difference. Lex Wunderink published a randomized study that showed better long-term outcomes for those patients who got off the medication or down to a very low dose. And so on: all of the study results published after 2010 simply provided more evidence that the use of antipsychotics needed to be rethought.
The recent study by epidemiologists at Columbia University and City College of New York, which led them to conclude that there isn’t good evidence showing that antipsychotics provide a long-term benefit, is simply one more data point in that larger body of evidence. Their study didn’t involve an assessment of the benefits versus risks of antipsychotics; rather they conducted a search of the literature to see if there was evidence that the drugs provided a long-term benefit, and in particular, whether the drugs reduced the chronicity of psychosis over the long-term. But they didn’t find evidence that the drugs were effective on this target symptom over the long-term, and that is why I titled my blog, “Timberrr! Psychiatry’s Evidence Base For Antipsychotics Comes Crashing to the Ground.” The relapse studies don’t provide evidence for their long-term use, and these researchers couldn’t find any alternative evidence that the drugs improved long-term outcomes.
So, as Allen Frances asked me to do, I have made my thoughts known. I do not think antipsychotics are “good” or “bad.” Instead, I think the scientific literature argues for a dramatic rethinking of their use, organized around two principles:
- Try to avoid immediate use of neuroleptics in first episode patients, as there will be a significant percentage who will recover without the medications (but aided by other forms of treatment), and this is a good outcome for those patients.
- Once the medications are used, there should be an effort to minimize their long-term use, with regular support for drug-tapering protocols.
Now, as Sandy Steingard has written, incorporating those principles into clinical care may be quite difficult. But if psychiatry is going to be “evidence-based” in its practices, and if it is going to put the interests of its patients first, then I believe it has a duty to develop selective-use protocols, which seek to minimize long-term use of antipsychotics (and other psychiatric medications). I also believe that our society should provide the resources to enable this rethinking of the drugs.
This is Not a “Middle Way”
In his Huffington Post blog, Allen Frances argues for prescribing practices that he describes as a middle way. Prescribe them to the right patients, because for these patients the drugs can be life-saving, but curb the overuse and polypharmacy that can prove harmful to so many, particularly for those who have ordinary problems, as opposed to real psychiatric disorders. As you can see in his blog, he also sees this middle way as informed by his own clinical experience.
But, here’s the rub: the “middle way” he describes is not an evidence-based practice. It is not a practice that is informed by science that tells of drugs that induce a dopamine supersensitivity, which may increase the biological vulnerability to psychosis; or of science that tells of drugs that shrink the brain, with this shrinkage associated with worse negative symptoms and functional impairment; or of animal research that tells of why antipsychotics fail over time; or of science that tells of much higher recovery rates over the long term for unmedicated patients. Those are drug effects that are not immediately visible to the clinician, but rather are made known through the illuminating powers of science, and they pertain to those with “clear cut psychiatric disorders” too.
I know this blog is ridiculously long. But climbing out of a pigeonhole, while trying to explain one’s thinking on a complicated topic, can be a laborious thing to do.
This blog first appeared on the author’s website, Mad In America and is reprinted with his permission.



